PM is key to the lower extremity. The association of PM with sciatic and other nerves in the gluteal area makes PMS a very frequent pathological condition. In fact, every abnormality on the lower extremity, from the thigh down to the foot (from active trigger points in hamstring muscles to Plantar Fasciitis), may be directly connected to PMS.
This article consists of three parts. Part I will review the anatomy and physiology of PM, Part II will present the evaluation of the patient with tension in PM and Sciatica, and Part III will show the entire MEDICAL MASSAGE PROTOCOL in cases of PMS.
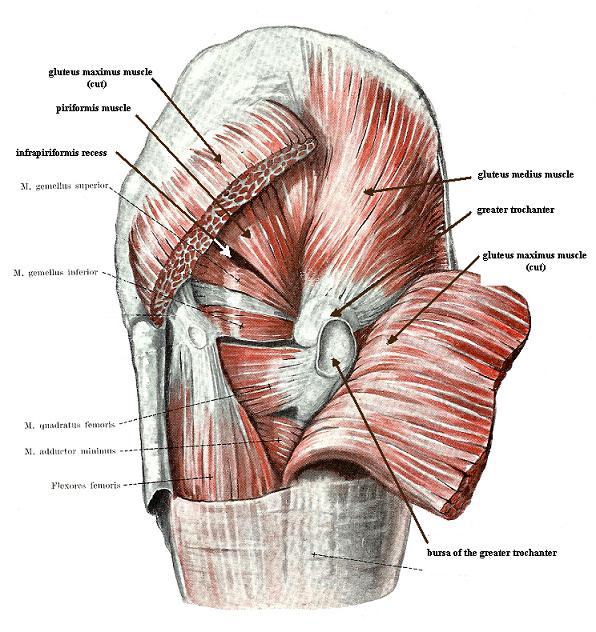
The PM originates inside the pelvis on the anterior surfaces of the sacrum, and the sacroiliac joint exits the pelvis via the greater sciatic foramen and inserts it into the greater trochanter (see Fig. 1).
a
b
Fig.1. Anatomical arrangement of the PM
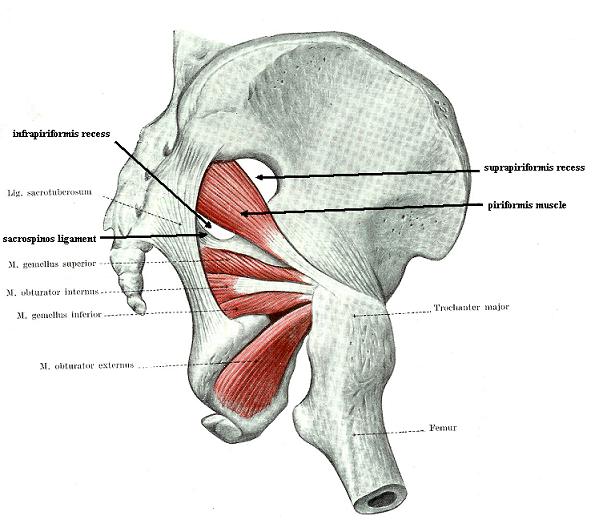
The greater sciatic foramen is formed anteriorly and laterally by the ilium bone, medially by the sacrum, and inferiorly by the sacrospinous ligament (see Fig 2).
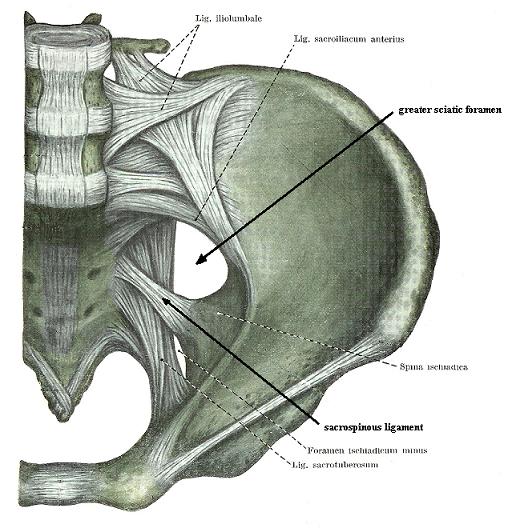
Fig. 2. Greater sciatic foramen
When the PM leaves the pelvis, it divides the greater sciatic foramen on the suprapiriformis recess and the infrapiriformis recess (see Fig. 1b).
In some individuals, especially those who build up the PM in the gym or during a professional sports career, the PM may occupy the entire greater sciatic foramen to the degree of eliciting pressure on neurological and vascular structures located in this anatomical opening (Ripani et al., 2006). The PM receives motor innervation from the S1-S2 spinal nerves.
The PM participates in the abduction and lateral rotation of the hip joint. The gluteal muscles, including the piriformis and quadratus lumborum muscles, are key players in our ability to walk upright. Every time we lift a foot to take a step, the opposite side quadratus lumborum muscle binds together the thoracic cage with the pelvis, and at the same time, the entire gluteal group stabilizes the hip joint. With such simultaneous action, the opposite side of the body becomes a rigid structure that acquires enough stability and balance to resist the force of gravity while we finish the step and are on both feet again.
Let’s look at the anatomy of the gluteal muscles. It is noticeable that all of them originate from the outer surface of the pelvic bones and sacrum and are inserted into the greater trochanter (see Fig. 1a). Only the PM starts from the inside of the pelvis (see Fig. 1b) and uses the same area of insertion (i.e., greater trochanter).
Although the PM’s action is similar to that of the other gluteal muscles, it is the only biomechanical force that stabilizes the hip joint from the inside of the pelvis and balances the action of all the other gluteal muscles. This is what makes the PM’s action unique.
Unlike other gluteal muscles, the PM is able to participate in lateral rotation and abduction in the hip joint, while the prime movement of other gluteal muscles is mostly lateral rotation.
The PM has one more unique biomechanical characteristic. It can elicit direct pressure and rotation force on the sacroiliac joint (Retzlaff, 1974). This fact greatly contributes to the tension in the SI joint and lower back pain {forms} as a result of Sacroiliitis.
The PM is an absolutely unique muscle in our body because of its complex relationship with many important nervous and vascular structures in the pelvis and gluteal area. Tension in the PM may affect the following structures.
1. Sacral Plexus
As discussed above, the inner third of PM is inside the pelvis. In the place of origin (anterior surface of the sacrum and SI joint), the PM forms a cushion for the sacral plexus, especially for S2-S3 spinal nerve roots (Russell et al., 2008). This plexus originates from many nerves (i.e., sciatic, gluteal inferior, cutaneous posterior, etc.) that innervate the pelvic inner organs, the gluteal area, and the lower extremities. Fig. 3 presents the anatomy of the sacral plexus and its relation to the PM borders, emphasized by solid red lines.
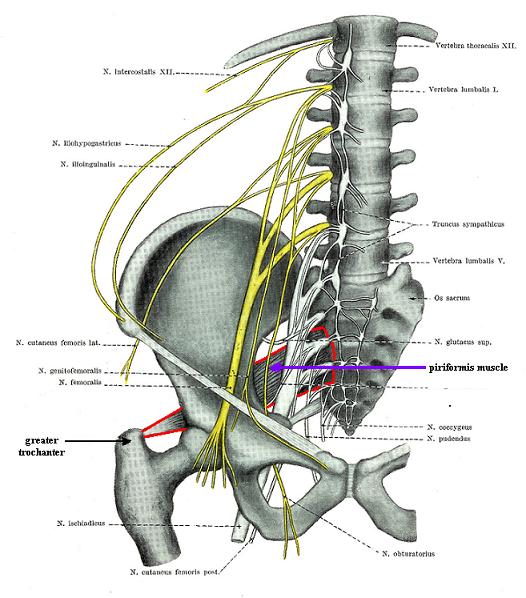
Fig. 3. Sacral plexus and PM
Clinical importance: If the PM gets tense, the sacral plexus loses its soft support, and symptoms of irritation may develop. The patient will exhibit a great variety of clinical signs and symptoms because the sacral plexus is the origin of the majority of peripheral nerves, which supply the pelvis and both lower extremities.
The clinical signs of the sacral plexus irritation by the PM are a unique combination of lower back pain, peripheral symptoms in the lower extremity, and a variety of visceral symptoms (e.g., constipation, intense menstrual pains, erectile dysfunction, etc.).
2. Sciatic Nerve
PMS is the major cause of Sciatic Nerve Neuralgia (SNN). The sciatic nerve is composed of two nerves: the tibial nerve (the anterior portion of the L4-S3 spinal nerves) and the common peroneal nerve (the posterior portion of the L4-S2 spinal nerves).
The sciatic nerve’s position in relation to the PM varies. Beaton and Anson (1938), in their classical study, examined 2250 cadavers and found that the sciatic nerve has the following major pathways regarding the PM.
1. In 85% of the population the sciatic nerve has the most common route when entire nerve exits the pelvis via the infrapiriformis recess, i.e. it is located below the PM (see Fig. 4 ‘a’).
2. In 10% of the population, the tibial portion of the sciatic nerve passes below the PM while the common peroneal portion penetrates the PM (see Fig. 4 ‘b’).
3. In 2-3% of the population, the tibial portion of the sciatic nerve passes below the PM, while the common peroneal portion of the sciatic nerve passes above the PM (see Fig. 4 ‘c’).
4. In 1% of the population, both portions of the sciatic nerve penetrate the PM (see Fig. 4 ‘d’).
5. 1-2% of the population exhibit less frequently occurring pathways
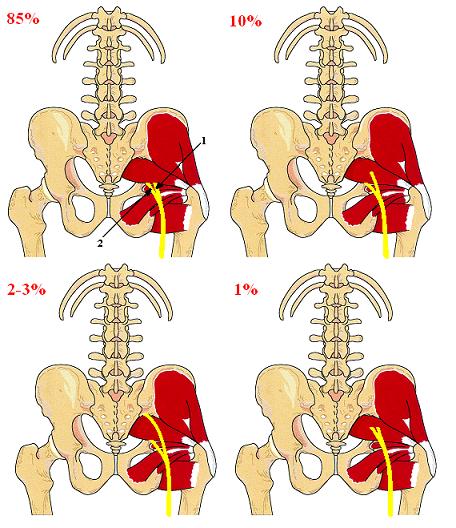
Fig. 4. Sciatic nerve and PM (from Travel and Simmons , 1983)
1 – common peroneal portion of the sciatic nerve
2 – tibial portion of the sciatic nerve
As you may see from Fig. 1 the common peroneal portion of the sciatic nerve is more frequently in trouble. This is why patients with PMS are more likely to develop sensory and motor abnormalities within the distribution of the common peroneal nerve (Lee and Tsai, 1974; Limansky, 1988). However, both portions or only the tibial nerve portion can also be entrapped. For those patients, the clinical picture of Sciatic Nerve Neuralgia is much more intense, and they struggle with constant flare-ups during their entire life.
3. Gluteal Nerves and Arteries
The superior gluteal nerve and artery exit the pelvis via the suprapiriformis recess. The inferior gluteal nerve and artery exit the pelvis via the infrapiriformis recess. The superior gluteal nerve innervates gluteus medius, gluteus minimus and tensor fascia latae muscles.
The inferior gluteal nerve innervates the gluteus maximus muscle.
Clinical importance: irritation of the gluteal nerves is accompanied by the formation of the active trigger points, protective muscle tension and weakness in the gluteal muscles.
The clinical sign of the inferior gluteal nerve neuralgia is weakness or complete inability (in cases of complete palsy) to get up from the seated position.
The clinical sign of the superior gluteal nerve neuralgia is an unusual rolling gait. Every time one raises foot on the unaffected side to make a step the half of the pelvis on the affected side slightly goes downward instead of being on the same level. The rolling gait is especially visible if the examiner gets on one knee to bring his or her eyes to the level of the patient’s pelvis and asks the patient to walk slowly while observing the gait from the back and comparing both sides.
4. Pudendal Nerve and Artery
The pudendal nerve is a major source of innervation of the sexual organs in males and females. It innervates the penis, scrotum, clitoris, and labia, as well as the anal sphincter and urethral sphincter. Finally, pudendal nerve contributes to the innervation of the skin on the posterior thigh.
Clinical importance: irritation of the pudendal nerve is a direct cause of sexual dysfunction in men and women (e.g., erectile dysfunction, dryness of the vagina, pain during intercourse, etc.) and sensory abnormalities (e.g., tingling, numbness) on the posterior thigh.
Part I of this article aims to illustrate that PM is a critical player in the human body, and any, even the slightest, pathological changes in its function cause a rich neurological picture in the pelvis, gluteal area, and lower extremities. In other words, the PM is key to the pelvis and lower extremities, and the practitioner’s ability to handle the tension in the PM greatly contributes to the overall success of the therapy of a variety of somatic and visceral symptoms in the lower back, pelvis, and lower extremities.
Part II of this article in the next issue of the Journal of Massage Science will cover evaluation of the client with tension in the PM and symptoms of Sciatica.
To become a Medical Massage practitioner, consider joining the Science of Massage Institute’s Certification Program:
https://www.scienceofmassage.com/seminars/
Beaton L.E., Anson B.J. The Sciatic Nerve and the Piriformis Muscle: Their Relationship a Possible Cause of Coccygodynia. J. Bone Joint Surg, (Br) 20:686-688, 1938
Lee C.S., Tsai T.L. The Relation of the Sciatic nerve to the Piriformis Muscle. J. Formosan Med Assoc., 73:75:75-80, 1974
Lymansky Y.P., Macheret E.L., Vaschenko E.A. The Neurological Symptoms of the Spodylosis. ‘Zdorovie’, Kiev, 1988
Retzlaff E.W., Berry A.H., Haight A.S., Parente P.A. The Piriformis Muscle Syndrome. JAOA, 73:799-807, 1974
Ripani M., Continenza M.A., Cacchio A., Barile A., Parisi A., De Paulis F.The Ischiatic Region: Normal and MRI Anatomy. J. Sports Med Phys Fitness, Sep, 46(3):468-475, 2006Russell J.M., Kransdorf M.J., Bancroft L.W., Peterson J.J., Berquist T.H., Bridges M.D. Magnetic Resonance Imaging of the Sacral Plexus and Piriformis Muscles. Skeletal Radiology, Aug, 37(8):709-713, 2008 Travell J.G., Simons D.G., Myofascial Pain and Dysfunction, The Trigger Point Manual, 2nd Edition. Lippincott, 1983.
Category: Medical Massage
