The purpose of this section of the Journal of Massage Science is to inform the practitioners about valuable articles that frequently go unnoticed, as well as to point to those authors and publications who present very questionable views in their writings. We do not play politics and we are not associated with any publishing company or professional association. We are a completely independent voice and we promise you direct unbiased reviews based strictly on the science.
If the author of the reviewed article does not agree with our opinion, we will be more than happy to publish his or her response and have a productive discussion over the article’s subject.
At the end of the year we will recognize and reward the author of the most important publication(s) and point to the authors of the most unscientific publication(s). We hope this will help to raise the bar of published materials in massage journals for the benefit of the entire profession.
Massage Today



Treatment Decisions for Peripheral Neuropathy. Massage Today April, 2012, Vol. 12, Issue 04, by Rita Woods, LMT
Compared to the last article on this subject, which we reviewed in issue #2 ofJMS, Part 3 is much better. It says less about treatment options and primarily concentrates on the theoretical aspects of peripheral neuropathy. The author deserves credit for mentioning that one of the side effects of cholesterol-lowering drugs is peripheral neuropathy. Considering the widespread prescribing of statins, more and more people are reporting symptoms of neuropathy.


Current Trends in Relieving Migraine Pain. Massage Today April, 2012, Vol. 12, Issue 04, by Kelly Lott, LMT, MTI, NCBTMB, CIMI
The article has an impressive title but, unfortunately, it only partially delivered what it promised. As “current trends” the article mentions medications, acupuncture and cold-stone placement. Considering that massage therapy was not even mentioned, it seems that according to the article published in Massage Today, massage therapy is not a current trend anymore.
It seems that the author is not aware that while she does not consider the massage therapy a valuable treatment option, recent medical sources do. According to several articles (e.g., Zanchin et al., 2001; Piovesan et al., 2009), published in such respected medical journals as Headache and Cephalalgia, which are world-leading medical sources on this matter, massage therapy, in fact, is one of the critical treatment tools to help patients with migraine.
According to the article, the placement of cold stones on the face will relieve such a complicated pathology as migraine. What is needed is to relieve the greater occipital nerve from pressure, restore mobility of the cranial aponeurosis or decrease the activity of trigeminal nerve in cases of cluster headaches (see article in Issue #2 and this issue of JMS). The author asserts that all these medical massage techniques are easily substituted by cold stones, which uses the simple fact of counter irritation.
It seems to us that many authors as well as publications live in some kind of bubble, which allows very little room for massage science, and continue to voice the same mistakes and incorrect views over and over again.
Zanchin G; Maggioni F; Granella F; Rossi P; Falco L; Manzoni GC. “Self-administered pain-relieving manoeuvres in primary headaches.” Cephalalgia, 21(7):718-26, 2001.





Tissue Density’s Relationship to Pain and Dysfunction. Massage Today April, 2012, Vol. 12, Issue 04, by Linda LePelley, RN, NMT
The reader may notice that this article has an unusual rating. Let us explain why. The article is devoted to the relationship between tissue density and pain. Indeed, this is an important topic. Here is a quote from the article, which tries to explain the formation of “muscle knots,” “tight” muscles and “trigger points.”
“My thoughts regarding the etiology of elevated TD involve the lipid-rich components of our extracellular fluids, which I believe are attracted to the bio-polymeric nature of our cartilaginous tissues. This attraction, combined with a variety of dynamic factors, including body heat, compressive force, overuse, injury, hypo-hydration, torsion, sheer force, tensile force, inertia, chemical environment and fluid viscosity may cause the extracellular fluid to accumulate, thicken and eventually precipitate into gelatinous plaque. Over time, I believe that these plaques harden and become mineralized, turning into the rubbery nodules…”
Yes, in the area of hypertonic muscle abnormalities, the tissue density increases in different degrees. All these “knots,” “points,” etc., have their own medical definitions, and it is time for practitioners use them and understand what they are dealing with. Increased tension in the muscles goes through three stages: formation of hypertonus, development of trigger points within hypertonus and substitute the hypertonus with trigger point by proliferated connective tissue to form myogelosis (to read more, please see the March-Aril 2009 Issue of JMSand read the article, “Science of Trigger Point Therapy”).
The author of this article considers that “…lipid-rich components of our extracellular fluids…” are the first stepping stones in the formation of “knots” and “points”. However, this is completely incorrect since the first morphological stepping-stone in the formation of “knots” (i.e., myogelosis) is deposit of glycoproteins in the areas of local ischemia. In such case, lipids have nothing to do with the formation of “knots.” It is sad that this simple fact, which has been known to medicine since before World War II, is still being debated in the 21st century in massage publications. This is why the article has two bad apples.
For the first time in four years of reviewing articles in major massage publications, we encountered the words: “My thoughts regarding….” In many instances, we read articles that leave us stunned and additionally their authors neglect to inform readers that this is their own personal opinion. Instead, they present information as a well-known scientific fact that in reality has nothing to do with medical and massage science. Here are several the most notorious examples:
Freeing the Heart, Part III: Elongating the Esophagus. Massage Today, February, 2012, Vol. 12, Issue 02, by Dale G. Alexander, LMT, MA, PhD. Our review published in #2 Issue of 2012
Auth Method. Addressing Root of Back and Shoulder Pain. Massage & Bodywork Mar-Apr: 62-67, 2011, by Shari Auth. Our review is published in #2 issue of 2011
Working With Headaches. Techniques for Migraines. Massage&Bodywork Magazine, Nov-Dec, 108-115, 2010, by Til Lichiau. Our review was published in November/December issue of 2010
Contrary to these publications, the author made mistakes, but she at least has enough courage to publish her article in discussion mode and for this approach, we are sure that she deserves our recognition. This is why in this particular case we used a double rating system.





Freeing the Heart Part IV: Reducing Resistance to the Heart’s Expansion.Massage Today April, 2012, Vol. 12, Issue 04, by Dale G. Alexander, LMT, MA, PhD
As we mentioned above, many massage educators live in a bubble that separates them from the reality of medical and massage sciences and is filled with their personal opinions. As a result of such an unfortunate situation, the practitioners who read such articles stay in that same bubble, which restricts the development of the profession or sends it in a completely wrong direction. This article is a great example of this scenario.
The article is a unique piece. The author mixes correct information with complete nonsense and presents the entire article in a query mode by asking questions in a discussion mode and immediately answering them. By twisting science and using excellent psychological maneuvers, the author imposes his incorrect views on the readers.
We reviewed Part III of this article in a previous issue of JMS (please clickhere). We are still stunned by unique and totally anti-scientific and anti-anatomical assumptions presented by the author. For example, he states that gastric juice from the esophagus leaks into the heart causing cardiac arrhythmia; or that the vagus nerve is affected by tension in the sternocleidomastoid muscle, etc. We provided all necessary data and pictures in the previous review. Part IV is another masterpiece of misinformation. Let us quote:
“The intimacy of the anatomical enfolding of the heart around the esophageal tube is a related variable; structurally, if the esophageal fibers are contracted or go into spasm and, as a chemical irritant, when chronic gastric reflux is considered. Since no one pays attention to such variables, this might be one way that we may contribute to our clients’ quality of life, as well as to possibly slowing the advance of cardiovascular disease.”
Is there no one at Massage Today who cares about basic anatomy about which the author definitely lacks knowledge? The esophagus is located in the posterior mediastinum, and the heart does not enfold it. The heart is in the anterior mediastinum and lies in front of the esophagus while each anatomical structure has its own system of fascial support. In addition, the heart is protected by the pericardium that safely guards it from the outside environment. I would like readers to pause for a second and imagine how, according to the author, no one in cardiology or gastroenterology thought about chronic gastric reflux affecting the cardiac function by triggering cardiac arrhythmia until Mr. D. Alexander started to think about it and made such a “valuable” discovery.
Now, let us give you the scientific data on the topic. According to Jaspersen (2006), who reviewed modern scientific data on the so-called ”extraesophageal” manifestations of acid reflux, this list includes:
1. Laryngitis
2. Hoarseness
3. Chronic cough
4. Asthma
5. Non-cardiac chest pain
Did any reader find in this list any forms of cardiac arrhythmia or insufficiency of coronary circulation Mr. Alexander tries to link with acid reflux? How can someone write and someone publish such ridiculous ideas that completely disregard the basics of medical anatomy, physiology, gastroenterology and cardiology, and rely simply on personal opinion without any supporting scientific data?
Here are another two quotes:
“Another implication of such strain along the length of the esophagus is that its tension can literally pull the head down upon the neck and is an influence contributing to the head being pulled forward which will inevitably activate the extensor reflexes of the spine. Might this be related to your client’s chronic neck and upper back pain? Let us remember that the superior sympathetic ganglia and the vagus nerve have their most intimate communication between the occipital and the 1st cervical vertebra, the atlas.”
And:
“How many of your clients (with cardiac or esophageal abnormalities by JMS) present to you with pain and muscle spasm between their shoulder blades?”
If the author just tried to learn at least the basic concept of medical massage, he would discover a completely different explanation to the fact that patients with esophageal and gastric abnormalities frequently have somatic abnormalities in the middle back. As Dr. Glezer and Dr. Dalicho showed long ago in 1955, patients with chronic gastric and esophageal abnormalities have tension in the soft tissue between the shoulder blades because this area shares the same innervation with the stomach and esophagus. Thus, somatic abnormalities in the form of muscle tension in this area are not the result of a short esophagus – which according to the author somehow pulls the head forward-but rather the result of reflex zones formation in the soft tissues.
The final issue is the vagus nerve. It appears the author desperately needs to prove that his treatment is effective, and he only can do that only by including the vagus nerve in his treatment since this nerve controls cardiac, esophageal and gastric functions. In Part II of this article, he stated that the vagus nerve is irritated by sternocleidomastoid muscle, and that his therapy frees nerve from irritation or compression. We reviewed the details of this “new anatomical discovery” in Issue #2, JMS, 2012. Now, in Part III of Alexander’s article, he states:
“Let us remember that the superior sympathetic ganglia and the vagus nerve have their most intimate communication between the occipital and the 1st cervical vertebra, the atlas”
Therefore, in two places in the same article, Mr. Alexander has placed the vagus nerve in two completely different anatomical locations! Mr. Alexander acknowledged the crucial importance of the vagus nerve as a major nervous pathway to control inner organs in thoracic and abdominal cavities. This importance is why the vagus nerve is hidden deep in the body, and has no significant obstacles along its route. However, in his article, Mr. Alexander has created imaginable obstacles to justify his therapy treatment. Unfortunately, no one prevented him from publishing this and subsequently misleading practitioners.
Jaspersen D. “Extraesophageal manifestations in gastroesophageal reflux disease.” Minerva Gastroenterol Dietol, 2006 Sep; 52(3):269-74. Review.




Infant vs. Pediatric Massage: What’s the Difference? Massage Today May, 2012, Vol. 12, Issue 05, by Tina Allen, LMT, CPMMT, CPMT, CIMT
A very good article that provides the basic definition of infant and pediatric massage. At first after reading the title of the article, we had our doubts about the value of putting infant massage versus pediatric massage since the infant period of development is part of pediatrics. However, the author made great efforts to explain and justify such distinction, and we agree that she has, in fact, made a very strong point. The article is especially informative for those practitioners who plan to expand their practice in this direction.





Exploring the SI Joint. Massage Today May, 2012, Vol. 12, Issue 05, by Whitney Lowe, LMT
Excellent article! Thank you!





Scalene Muscles: Playing Havoc with Your Clients. Massage Today May, 2012, Vol. 12, Issue 05, by Nicole Nelson
A very good article on a hugely important topic. The anterior scalene muscle is a key to the upper extremity, and has the nickname “silent killer” since it can trigger any abnormality in the upper extremity without patients complaining about pain on the anterior or lateral neck. We may only add to this article that blending Postisometric Muscular Relaxation into the discussed protocol would greatly speed up treatment and help achieve stable clinical results.

What You Should Know About Corticosteroids. Massage Today June, 2012, Vol. 12, Issue 06, by Rita Woods, LMT
A good article on the side effects of corticosteroid therapy, how it affects the client’s body and what practitioners should consider when working on a client who undergoes such treatment.
However, in this article the author again delivers the same harmful recommendation she already made in her previous publication, which we reviewed in issue #2 of JMS 2012 (click here). Here is her quote from this article:
“So, even if your client is undergoing chemotherapy and suffering with chemotherapy induced peripheral neuropathy, the deeper work on the feet to address this issue is generally acceptable.”
We have already discussed this issue in Issue #2, 2012 of JMS and provided references to show that this position is harmful to patients. We would like to ask the author one simple question: “Who exactly generally accepted the fact that deep tissue work should be used on patients with peripheral neuropathy developed as a result of chemotherapy?” We think that practitioners are entitled to know this since we have shown, based on medical sources, that this recommendation is dangerously incorrect.


Achilles Tendon and Foot Pain Caused by Tibialis Posterior. Massage TodayJune, 2012, Vol. 12, Issue 06, by David Kent, LMT, NCTMB
Overall, this is a very good article on the treatment protocol for tension in the tibialis posterior muscle. The author also provided videos that illustrate each step he suggests. There are two issues we would like to address here since they are missed or incorrectly presented.
In Step 2, which the author called Pincer Compression, he advocated deep compression in the middle of the leg between both parts of gastrocnemius muscle and soleus muscle. Click here to review the video. The idea of this “therapy” is to reach the posterior compartment of the leg muscles where the tibialis posterior is located.
Let us briefly look in the basic anatomy of this area. As you may see in Fig. 1, the gastrocnemius and soleus muscles are exactly in the middle of the posterior leg, where the article suggests the application of compression. The tibial nerve is located in the soleus canal together with tibialis posterior artery.
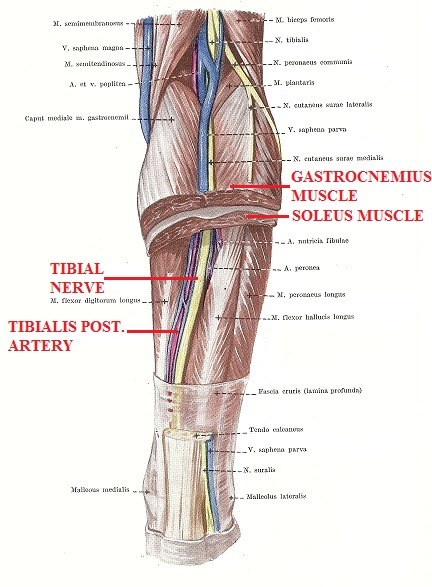
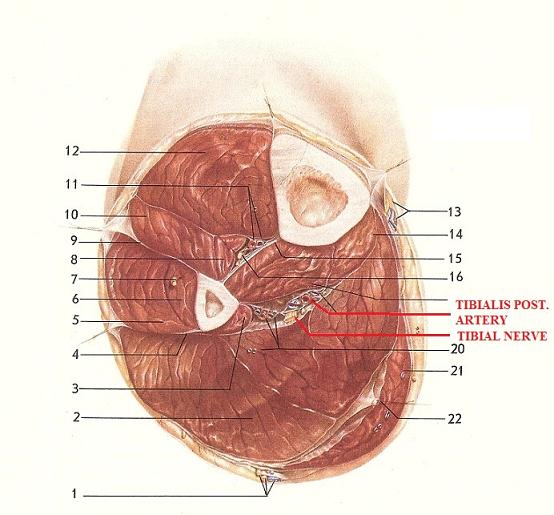
Now, if you look at Fig. 2, which illustrates the cross section of the leg, you will see that the tibialis posterior muscle forms a cushion for the tibialis nerve and tibialis posterior artery since this muscle is located under the nerve and the artery. Thus, application of compression as it is suggested in the article and shown in the video will directly endanger the tibial nerve and tibialis posterior artery because the practitioner will compress them against the tibialis posterior muscle and the tibia bone itself. The practitioner should work in the soleus canal when needed but instead of the compression he or she should apply longitudinal and cross fiber friction. In such a case the pressure will have a horizontal application instead of vertical compression.
The second issue, which the article misses, is the fact that if there is no direct trauma or any significant overload to the leg, the real cause of tension and active trigger points in the posterior tibialis muscle is irritation of the sciatic nerve or, more precisely, its tibial portion in the lower back or gluteal area even if patient does not complain about any uncomfortable sensations in these area. In such cases, for tension of the tibialis posterior muscle, the recommended protocol is useless since the real cause is not the tibialis posterior muscle itself but the origin of its innervation. Until the tibial nerve is released from the pressure in the upper parts of the body, the local treatment of the tibialis posterior muscle is a waste of time and the patient’s money.
Massage & Bodywork Magazine





The Long and Short of It. Strategies For Softening Tight Muscles. Massage & Bodywork May-June: 29-30 2012, by Art Riggs
A short but very well presented and articulated article. Considering the complexity of the issue, the author was able to answer the original question while clearly stating that his answer and position covers only part of the topic.





Scalenes. Massage & Bodywork May-June: 45-46, 2012, by Christy Cael
The author hosts a column in which she tries to teach practitioners how to palpate various muscles in the body. In many cases, her articles fail on this very simple subject. Unfortunately, this article follows the same pattern. The author states:
“The scalenes consist of three parts: anterior, middle and posterior. Each portion has vertically oriented attachments on the cervical transverse processes which then spread horizontally prior to inserting on the ribs.”
First of all, there are four scalene muscles: anterior, middle, posterior and minimi. Secondly, they are not portions but individual muscles that have their own origins and insertions. The author is supposed to know or verify such basic information, which can be found in every anatomy book, before writing her article. The difference between the individual muscle and portions of the same muscle is that in the first case the muscles (e.g. scalene) have an individual origin and insertion, while portions of the same muscle share the same origin and insertion (e.g. trapezius or quadratus lumborum).
Now let us get to the palpation portion that is the main goal of the article. Despite the text correctly describing the place of the palpation, the picture completely misleads the reader. It seems that the text was taken from a textbook but the author personally does not know how to find the correct location of the scalene muscles on the human body. This lack of anatomical knowledge explains the incorrect picture, which shows palpation of anterior scalene muscle whereas the article is describing the palpation of the sternocleidomastoid muscle. In the picture (to view please click here), the client is lying supine with his head in the middle position. This is the first mistake since in this position, the sternocleidomastoid muscle covers the scalene muscles and effective palpation becomes impossible. In the picture, the practitioner’s third finger of the right hand, which she uses for the palpation of the right anterior scalene muscle, is placed under the lower jaw in front of the angle of the mandible. In the article, the author correctly writes that the scalene muscle originates from the transverse processes of the cervical vertebrae. Could the author explain in such case how she was able to find the transverse processes of the cervical vertebrate under the lower edge of the mandible? If the author cannot match the text from the textbook with the body of the client, she should enroll in an anatomy dissection class before she writes such misleading information.
We expect that some readers may say that it is not important if the author placed the examining fingers slightly anteriorly. However, in this particular case, the palpation advocated in the article may have serious complications. Examine the picture carefully and you may notice that the third finger, which is supposed to go down to palpate the scalene muscles as it presented in the picture will go along and in front of the sternocleidomastoid muscle, which is palpated below the lower edge of mandible. With such palpation going down, the practitioner will get to the area of carotid sinus and palpation of carotid sinus may trigger a sudden drop of arterial pressure to the degree the client could pass out.
In cardiology, carotid sinus massage is a very effective tool to eliminate supraventricular tachycardia and restore normal cardiac (i.e. sinus) rhythm. Also, as it was correctly pointed by the April (1990), unnecessary palpation of the carotid artery and sinus is extremely dangerous in elderly patients since “atheromatous plaques may be dislodged to the brain” and cause a stroke.
Thus, in the picture that the author published and recommended to follow, she thinks that her palpating finger is on the anterior scalene muscle while it is really positioned on or superiorly to the sternocleidomastoid muscle and if goes down it will hit area of the right carotid artery and carotid sinus. Compare the location of the carotid sinus in the Fig. 3 with the direction of palpation the practitioner should follow presented in the picture from the article using the link provided above.
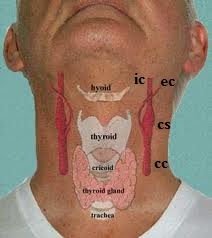
cc – common carotid artery
cs – carotid sinus
ec – external carotid artery
ic – internal carotid artery
By publishing this article, C. Cael and Massage and Bodywork Magazine set practitioners on a wrong and dangerous path. By the way, the homework stretch recommended to the clients is also incorrect.
The video below illustrates position of major anatomical landmarks and anterior scalene muscle on the right neck and correct head position for the palpation. In the video: the dot behind the ear indicates the mastoid process; dashed line – indicates the posterior edge of sternocleidomastoid muscle; two solid lines indicate the anterior scalene muscle; waved line indicates the clavicle.





Your Secret Weapon. 10 benefits of a Side-Lying Position. Massage & Bodywork May-June: 66-71, 2012, by Shari Auth
Ms. S Auth continues to misguide practitioners. First, it was a never-ending chain of articles in which she advocated that massage using only elbow and forearm is a solution for a successful massage practice in all fields from stress reduction to medical. Now she presents another erroneous twist: According to this article, massage therapy to eliminate pain and restore somatic function is conducted best with the client lying on his or her side. Here are the advantages mentioned in the article, and our comments from the basic logic absent in this article.
1. Client Evaluation
Quote:
“Side lying position is a great way to evaluate muscle tightness in your client because the therapist can move a client’s shoulders or pelvis forward, back, up, and down to feel for where the joint is impinged”
The readers of Massage and Bodywork Magazine and JMS are professionals. So, just from common sense, can someone justify the effectiveness of performing a clinical evaluation while the client lies on his or her side? In this position, the practitioner is unable to compare function or tension between affected and unaffected sides because the client is lying on the unaffected side. It distorts clinical evaluation and sends the practitioner in the wrong direction.
2. Troubleshooting
Quote:
“Because the whole shoulder griddle and pelvic griddle are available to be massaged in a side-lying position , troubleshooting pain is easier.”
Again, considering that as professionals, we know that lying on the side is an unbalanced position and it changes the normal biomechanics of the body and disturbs the balance between the right and left side, how can such nonsense be published in a national publication? Also, we would like to see the client with severe muscle spasms in the lower back placed on the side and being comfortable while the author sticks an elbow in various parts of the client’s lower back.
3. Balance and realign
Quote:
“… it is possible to balance the front of the joint respectively to the back of the joint and vice versa”
We have already discussed the matter of balance above. We just would like to mention that apparently restoration of the balance between both sides is not on the agenda of Auth’s method.
4. Stretch and Lengthen
Quote:
Side lying position gives “… more opportunities to stretch”
Yes, it is correct that the side position is used for some type of stretches, e.g., the quadratus lumborum muscle, but the author does not have the right to project this and other limited numbers of cases stating the side-lying position is necessary for the entire massage therapy session. How, for example, can the stretching of the lumbar erectors or posterior cervical muscles be done from the side-lying position in a balanced way, or perhaps the author does not address these areas at all? In the clinical setting, the side-lying position gives fewer opportunities to stretch.
5. Massage Lateral Side of the Body
This part of the article is correct if the patient is not in severe pain. For these patients it is impossible and clinically wrong to place them on their side.
6. Body Mechanics
Quote:
“Body mechanics experts are in favor of a side-lying position because it allows the practitioners to maintain a neutral spine while massaging”
This is quite a statement. We would like to have the names of the “experts” and references that the author consulted. There are no names just because no expert with a clear mind would suggest that working on the side-lying client is biomechanically better for the practitioner’s body.
Mrs. Auth suggests that the Auth’s Method consists of rubbing the elbow and forearm into the soft tissue and the fact that this will be easier to do on the client’s body if he or she is in the prone position because the practitioner may use body weight as an additional factor.
7. Client comfort
Quote:
“Side lying position is reminiscent of the fetal position and is the position many people sleep in.”
Yes, for some healthy clients the above can be true, but there are people who are more comfortable in the prone position. Should the practitioner force them into the side-lying position as an important component of a successful massage session?
However, the main goal of the article was to teach practitioners a better way of working with clients who are in pain. From this point of view, the side-lying position is unbalanced and generates pain. It seems that the author does not work on patients, for example, with Sciatica or Severe Trochanteritis, who only can be comfortable on their stomach with a pillow under the belly or on the back.
8. Clinical Advantage
This is our favorite one. Since the author was not able to find any argument to support the idea of the clinical advantage of the side-lying position, she simply stated:
“Learning to massage clients in a side-lying position will give you an edge over the competition because you will be able to treat a wider variety of issues more effectively.”
That is it – just get your client on a side, learn how to stick your elbow in various body parts and “you will be able to treat a WIDER variety of issues MORE effectively.” We would like to know what exactly the author compared Auth’s Method to: Neuromuscular Therapy or Myofascial Release or Segment-Reflex massage?
9. Forearm Massage
Only now do we get to the real goal of the entire article in which Ms. Auth successfully hid until now under the mask of providing practitioners with the miracle tool of laying the client on the side.
Quote:
“It’s possible to massage the whole body in the side-lying position using your forearms because forearms are more durable than the hands….”
Considering that it will be very difficult to use effleurage or friction or especially kneading in side-lying position, the only way to do it is with Auth’s method. Just learn how to do an hour massage using the forearm and elbow, disregard the science of massage with all its technical advantages and developments, neglect common sense and Auth’s method will save your hands and allow you to help everyone who is in pain. The only thing left is to register for the seminar conveniently provided at the end of the article.
10. Better Access
Ms. Auth is a prolific writer who cleverly promotes her agenda. In this part, she describes how easy it is to work on the tensor fasciae latae muscle while the client is lying on the side. This description is completely correct but she uses this treatment as an example of how to make wrong generalizations for the entire body and tissues, which are sometimes even impossible to reach from the side-lying position.
So, in reality, the article informs readers about 10 disadvantages of doing the entire massage treatment with the client positioned on the side instead of 10 benefits as stated in the title.





Bodyreading The Meridians. The Deep Front Line. Massage & Bodywork, May-June: 98-103, 2012, by Thomas Myer
As usual, a great article!




Cleaning Up Housekeeping Workers Injuries. Massage & Bodywork May-June: 104-107, 2012, by Whitney Lowe
This article is an overview of the most common injuries associated with housekeeping jobs in the hospitality industry. The author is completely correct when stating that massage therapy can be of great help for those workers but low wages prevent them from seeking massage practitioners’ help unless the medical office has a therapist on staff to work with medical insurances.





Interosseous Muscle Strain. Massage & Bodywork May-June: 108-111, 2012, by Ben E. Benjamin
A great and very informative article on the subject!




Working With Hammertoes. Massage & Bodywork May-June: 111-117, 2012, by Til Luchau
Overall, this is an excellent article that correctly educates readers about hammertoe deformation. We have two problems with it. First of all, the article correctly mentioned that the second toe is mostly affected with hammertoe deformation. However, in the majority of cases, the hammertoe deformation of the second toe is the result of Hallus Valgus or lateral deviation of the greater toe in which in tight shoes forces it under the second toe creating its hammer-like deformation. In such cases, the real cause is Hallus Valgus deformation that needs to be corrected first since this is the real cause of second toe’s problems.
The second issue is the clinical value of the recommended therapy. It gives the readers impression that manual therapy significantly helps clients with hammertoe deformation. However, this is not a case. Yes, manual therapy may to some degree help patients in the very early stages of deformation. However, as we discussed above, the hammer-like deformation of second toe is a result of Hallus Valgus, which very frequently is the case, and in these cases the techniques discussed in the article are a complete waste of time and patient’s money. As stated in the article:
“It also is reasonable to imagine that soft-tissue lengthening could, at least in some cases, delay or prevent surgery, and so avert the resulting loss of mobility that patients often experienced after corrective surgery”
First of all, this is an unfair twist of the clinical reality. Correctly conducted surgery on hammertoe does not cause a “…resulting loss of mobility that patients often experienced.” This is a very simple and effective surgery and the author’s statement is the fruit of his imagination.
Secondly, if the hammertoe deformation is moderate the surgeon may operate on the soft tissue only. If the patient waits too long and relies on false hopes as promised in the article, he or she wastes important time that may result in the patient requiring more extensive surgery on the bones with the increased potential of complications and a longer rehabilitation period.
Please remember all this before taking responsibility for hammertoe-deformation treatment. The discussed treatment is effective in the very early stages of deformation when the patient does not even think something is wrong with the toe(s). The practitioner may offer help if he or she detects such deformation and explains the importance of its treatment to the patient.
Separately, we would like to emphasize the fact mentioned in the article but we think may be overlooked by readers. The techniques discussed in the article are of significant help for those patients recovering after the surgery for the hammertoe deformation. This is the real value of the article and discussed treatment.
Massage Magazine


The Migraine Miracle. Massage Magazine 191, April, 2012: 62-66, by Kelly Lot
The article describes a method of migraine treatment that consists of massage therapy, cold stone application and aromatherapy. According to the article, this therapy has a miraculous effect for clients with migraines. We have no means to justify or deny these claims.
No one disputes the value of aromatherapy in stress reduction, various psychological abnormalities, etc. However, from our personal experience, we could tell that the proposed treatment for migraine sufferers may work only temporarily since it is based on sensory counter irritation rather than actual treatment (e.g., free the greater occipital nerve from the irritation). Also, a percentage of migraine sufferers experience the olfactory aura and aromatherapy is counter indicated for this group. This issue was not even mentioned.
Some other thoughts: Here is quote from the article:
“Each human cell has different tasks. Each cell has receptors…These natural receptors accept certain substances (aroma from the essential oils, by JMS) as friendly and pleasing. The body is naturally attracted to them in the attempt to return the body to its natural state of homeostasis,”
We think that the author as well as the publication must stoop to the use of groundless statements such as this one that misleads practitioners. What is the exact name of the receptors on each cell that the author knows, and we do not, that will alter the function of the cells after inhaling aromatic oils? We think that readers are entitled to that information, and if such receptors do not exist, then the author and the publication must be held accountable for the inaccuracy. If our cells are so vulnerable that they will easily change their function as a response to smell, we as a human race would have become extinct long ago.




Myofascial Release for Fibromyalgia. Massage Magazine 191, April, 2012: 50-54, by Richard Harty, PT
The article gives a general overview of Fibromyalgia treatment using Myofascial Release. In fact, this technique is supposed to be the first choice for the initial treatment of Fibromyalgia patients. We think that the article concentrated too much on the emotional component of the treatment while sacrificing practical recommendations, which can be used by readers the next day in the therapy room but this was the author’s choice.





Research. Review of two research papers: “Thermal Therapy Effects Lasting Improvement in Fibromyalgia” and “Massage Benefits Pediatric Transplant Patients.” Massage Magazine 193, June, 2012: 72-73
This research column in Massage Magazine is very helpful for practitioners since it keeps them updated on massage science. Both reviewed articles provide helpful information the practitioners may use to promote their services and help those in need. From our point of view, the Fibromyalgia article is especially important since it examined the effects of thermal therapy (sauna and exercise in a heated pool). In many clinical cases and articles on Fibromyalgia published in physical therapy and massage journals, the application of ice therapy is always one of the main treatment options. However, this approach is completely wrong for these patients and the reviewed research paper clearly proved that.
Additionally, exercise in the swimming pool is a powerful therapeutic pool for Fibromyalgia patients. We strongly believe that before the practitioner starts treatment of a patient with Fibromyalgia, the practitioner must insist on the patient start light, repetitive exercises in the water for a couple of weeks prior. These exercises will make a significant difference in the positive outcome of treatment since the absence of the force of gravity will increase blood flow to the affected areas, restore the balanced relationship between muscle synergists and antagonists as well as between the right and left sides.
However, one of the critical benefits of water exercise is an increase of muscle mass without triggering additional muscle spasms. Exercises with gravity, which are used as a treatment option for patients with Fibromyalgia, are an incorrect initial approach. Fibromyalgia is caused by an energy crisis where level of ATP, which is the main energy source for muscle contraction and relaxation, decreases. Therefore, exercises with gravity will use all available ATP for the contraction while little left for the relaxation resulting in additional muscle spasms.
Alternatively, water exercise for the Fibromyalgia patients increases muscle mass and is safer to use. This is why water exercises are such an important component of successful somatic rehabilitation. Because in the water muscles do not fight with the force of gravity, smaller amounts of ATP is used while muscle mass continues to increase safely without triggering additional muscle spasms.
This is why we greatly appreciate that Massage Magazine brought this research paper to the attention of practitioners.





Breast Cancer-Related Lymphedema. Role of Manual Lymphatic Drainage.Massage Magazine 193, June, 2012: 62-66, by Joachim Zuther
Simply an excellent article that we highly recommend reading and consider to learn Lymph Drainage Massage for these types of patients. It is a very simple truth: There is no any other modality in modern medicine that is able to help breast cancer survivors fight Post-surgical Lymphedema. This is where Lymph Drainage massage is an irreplaceable treatment tool!





Heart Health. Massage Therapy, High Blood Pressure and the Heart.Massage Magazine 193, June, 2012: 54-59, by Debra Curties
This is a very informative article on massage therapy as a treatment option for patients with Hypertension. It seems that the primary goal of the article is to give a general overview of the issue, and the author successfully accomplished that.
The main treatment goal mentioned in the article is to unload the heart by decreasing the peripheral vascular resistance. This is a correct and very valuable contribution of the massage therapy to the overall treatment of patients with Hypertension. We just would like to add another important aspect, which is the clinical effectiveness of MEDICAL MASSAGE PROTOCOL to control Hypertension by eliminating reflex spasms in the pool of vertebral arteries. Practitioners should consider this often frequently missed component of the massage treatment of patients with Hypertension.


Spontaneous Muscle Release Technique. Deep Tissue Work with Less Pain and Effort. Massage Magazine 193, June, 2012: 48-53, by Dawn Lewis
We would like to state at the very beginning that this approach to the treatment advocated in the article is correct. Successful somatic rehabilitation indeed requires a careful approach to the soft tissue without activating the pain-analyzing system of the patient. This recommendation is widely accepted by anyone who practices medical massage and manual medicine since the 1960s, after Professor Mezlack and Professor Wall formulated their famous Gate-Control Theory of Pain.
Overall, the “new” method developed by Lewis is a recycling of already very well known and for many years successfully used techniques, which are part of Myofascial Release and Muscle Energy Techniques.
We examined the proposed “new” method according to the information presented in the article. There is a chance that the author has developed a very advanced treatment method but does not want to share it with readers. However, the information in the article gives an excellent sense of the “new” therapy.
On the final note, why the use of “spontaneous” in the title? According to Merriam-Webster’s Dictionary, the definitions of “spontaneous” are:
1. Proceeding from natural feeling or native tendency without external constraint
2. Developing without apparent external influence, force, cause, or treatment
The treatment described in the article is application of external influences to the body including proprioreceptors, which according to the article the author is able to “speak to” (we took this terminology from the article). Let us for a second imagine the face of any health practitioner from PT to MD when, during an interview, the practitioner states that he or she practices “Spontaneous Muscle Release Technique.” It brings us to the same subject we discussed before: The absence of verified data on the science of massage therapy hurts the entire industry, and, what is more important, confuses practitioners. It is pointless when the same modalities are reused and called by different exotic names that sometimes do not even make sense.
Massage Therapy Journal





Orthopedic Assessment of Strains and Sprains Massage Therapy Journal51(2):74-80, 2012, by Dr. J.E. Muscolino
This very informative article discusses several simple tests to examine the degree and extent of soft-tissue damage. Besides informing practitioners about necessary tests, the author tries to teach readers how to analyze critically the obtained data. This is a great plus for the article.
Category: Good Apples, Bad Apples
