The purpose of this section of the Journal of Massage Science to inform the practitioners about valuable articles that frequently go unnoticed, as well as to point to those authors and publications who exhibit low educational standards. We do not play politics and we are not associated with any publishing company or professional association. We are a completely independent voice and we promise you direct unbiased reviews based strictly on the science.
We would like to clarify our position on articles of a promotional character frequently published in major massage journals. All promotional articles which deal with medical aspects of massage therapy are lamentably similar. They begin with how important the subject of the article is for the massage therapist; proceed with how to apply several diagnostic tests; and then provide only a very short description (if the reader is lucky) of how to actually fix the problem discussed in the article. The next step is to buy author’s video or book or enroll into his or her seminar.
One may ask, “What is wrong with articles intended to promote authors’ publications or seminars?” There are two points we wish to make in response to this question. Firstly, we feel there is nothing wrong with articles intended primarily to promote seminars, DVDs or books that deal with the general-health or spiritual aspects of massage or provide instruction on stress-reduction or therapeutic massage techniques. In our opinion, however, the situation changes completely if the author is presenting a new development or recommendation which he or she claims confers medical benefit to the client. In so doing, the author steps into different territory altogether, in which he or she ought, we believe, to be required to answer to the more stringent standard of medical publications.
Let’s imagine that a physician submits an article to a medical journal in which he stresses the significant incidence of inflammation of the knee, informs the reader of what the clinical symptoms are, and then proceeds to make reference to a new approach he has developed to cortisol injection into the knee — without providing sufficient information on how he executes his method of treatment. There is no medical publication in the world in which an article such as this would stand a chance of publication. Yet, we see such promotional articles in virtually every massage journal. In our view, there ought to be no difference in standard with regard to content requirement between a massage publication or a medical publication, where medical topics are concerned.
Secondly, we recognize that for many authors, it is proceeds from their books, DVDs and seminars which constitute the bulk of their living, and we are thus fully sympathetic to the needs of these authors to promote their contributions to the field. We are convinced, however, that even from a promotional standpoint, authors would invite greater response to their books, DVDs or seminars if, in their articles, they were instead to fully describe the treatment method the propose — to a level of detail and thoroughness allowing the practitioner to take the technique directly to the table, be impressed with its results, and be thus persuaded that the know-how of the author is definitely to be further sought out.
If the author of the reviewed article does not agree with our opinion, we will be more than happy to publish his or her response and have a productive discussion over the article’s subject.
At the end of the year we will recognize and reward the author of the most important publication(s) . We hope this will help to raise the bar of published materials in massage journals for the benefit of the entire profession.
MASSAGE & BODYWORK MAGAZINE




Sports Massage. 10 Winning Concepts. Massage&Bodywork Magazine, Nov/Dec: 23-25, 2014
By Rebecca Jones
The article is written in a journalistic format and gathered professional opinions on the issue of Sports Massage. It can be very helpful for those who would like to extend their practice into the Sports Massage field.
The author deserves credit for putting many correct components under the roof of one integrative approach to Sports Massage. Unfortunately, when one follows experts in Sports Massage it becomes obvious that separately they have tunnel vision promoting what they are trying to teach or sell (e.g., kinesio taping, massagers, sports massage seminars, etc.). Since the author is free from any monetary interest, her small article emphasizes an important point: success comes from a combination of factors rather than one silver bullet which doesn’t exist in real life.


Understanding Pain. Massage&Bodywork Magazine, Nov/Dec: 34-37, 2014
By Anne Williams
This is a very basic article on pain with many modern concepts of pain completely missed (e.g., Neuromatrix Theory of Pain). A very helpful part of the article is the
Table: Classification of Pain. Therapists may use this information for pain evaluation. We gave a complete overview of pain and its control by massage therapy in issues #3 and #4, 2014 and issue #1, 2015 JMS.



Amputation Adaptations. How Massage Therapy Can Help. Massage&Bodywork Magazine, Nov/Dec: 40-43, 2014
By Ruth Werner
The author deserves a lot of credit for raising this important topic. Massage therapy indeed is an extremely valuable tool for controlling phantom pains, taking care about the stump, addressing mental issues, etc.
We only wish the actual treatment recommendations were verbalized more precisely since that would make the article more valuable. Such information even deserves a separate section.




Biceps Femoris. Massage&Bodywork Magazine, Nov/Dec: 47-48, 2014
By Christy Cael
Good article on biceps femoris palpation.





Wounded Warriors. Massage&Bodywork Magazine, Nov/Dec, 2014
There are several articles on this subject in the Nov/Dec issue of Massage&Bodywork Magazine. We think the Editorial Board deserves a lot of credit for raising this issue and dedicating a large portion of the magazine to this topic.





Freeing the Quadratus Lumborum. Massage&Bodywork Magazine, Nov/Dec: 82-87, 2014
By Peggy Lamb
An excellent article on the quadratus lumborum muscle – its anatomy, function, testing and treatment protocol. The author, in contrast to many educators who exclusively promote various ‘mobilization’ and ‘stabilization’ techniques, understands this critically important basic: the tissues must first be treated manually before any other modalities are used.
Unfortunately, many therapists under the influence of incorrect teachings forget about this important basic and only stretch, mobilize, etc. Some of them don’t even call themselves massage therapists anymore since incorrect ideas were sold to them under the umbrella of superior training. Thank you for this important article!



Rebuilding Alan’s Thumb. Massage&Bodywork Magazine, Nov/Dec: 94-97, 2014
By Whitney Lowe
A good article on DeQuervain’s Disease. The illustrations are very helpful. However in the treatment part a very important component is missing. The clinical results of the therapy discussed in the article will be unstable since the same pathology will re-occur if the therapist doesn’t restore the anatomical length of the muscles, reset muscle spindle receptors and decrease pressure on their tendinous parts. In a sense, DeQuervain’s Disease is a consequence and treatment of the tenosynovitis itself without addressing the original cause isn’t enough.




Spring in the Arches. Active Movement Leads to Proper Alignment. Massage&Bodywork Magazine, Nov/Dec: 98-99, 2014
By Mary Ann Foster
A good article on foot biomechanics with helpful illustrations. Apparently this is the last contribution by the author to Massage&Bodywork Magazine and we wish her luck since her articles have contributed to the content of magazine.


Scoliosis: Fixed or Fixable? Massage&Bodywork Magazine, Nov/Dec: 100-101, 2014
By Erik Dalton
This is a small article on the very important subject of Scoliosis and how to address it with manual therapy. We couldn’t agree more with this beautifully stated sentence:
“…there is always a functional (fixable) component to every structural (fixed) scoliosis.”
In other words, with the correct therapy there is always the potential to decrease pressure within a curved spine and to some degree unwind deformation.
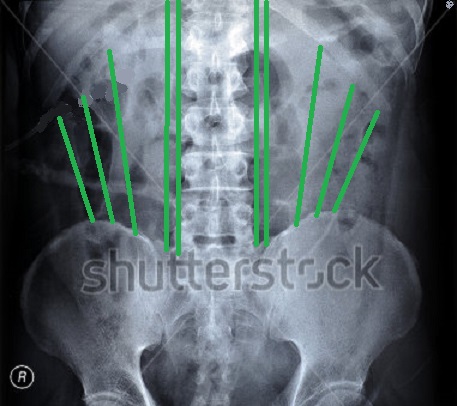
To fully understand this review we need to quickly look at major biomechanical changes in patients with Scoliosis. Let’s start with norm. Fig. 1 which shows an X-ray of a normal spine.
Fig. 1. X-ray of a normal spine with a normal distribution of tension
Green lines – balanced distribution of pressure between lumbar erectors (two parallel lines) and quadratus lumborum muscles (three slanted lines) on both sides
Fig. 2 shows the X-ray of two curves scoliosis with the right side thoracic curve of 70 degrees and the left side lumbar curve of 45 degrees.
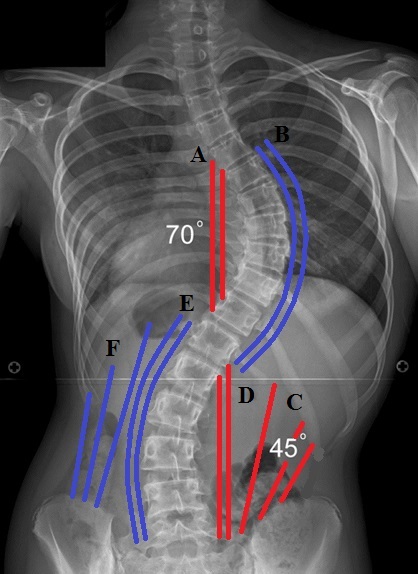
Fig. 2. Scoliosis and the main pattern of pressure distribution in the back muscles
Red lines – muscles in spasm and shortening
Blue lines – muscle weak and overstretched
Now let’s go over the pattern of pressure distribution. For the spine to function properly the force of gravity as well as muscle tension must be spread equally (see Fig. 1). In cases of scoliosis everything is dramatically changed. There are so many pathological changes in the body of patients with scoliosis, from feet to the shoulders, that we can address here only its main component: abnormal pressure distribution in the back muscles.
Look at Fig. 2. The paravertebral muscles on the right middle back (B) which are on the convex side of the thoracic curvature are weak and overstretched. They are desperately trying to resist the pressure build up in the concave side by the left paravertebral muscles (A) which are short and spastic.
Additionally the right quadratus lumborum muscle (C) is short and pressured since it developed the habit of functioning when the thoracic cage and pelvis are drawn closer to each other.
The situation is mirror-like in the lumbar curvature. Here we can see that the right lumbar erectors (D) are short and spastic while the left lumbar erectors (E) are weak and overstretched. The left quadratus lumborum muscle (F) shares the same destiny. It is also weak and overstretched.
In a patient with scoliosis the A and D areas act as a string for the bow. The more pressure that develops in the string the more progress of the curvature and weaker muscles on the opposite side.
Let’s keep Fig. 1 and Fig. 2 in mind and move to the treatment options discussed in the article. Yes, the article mentioned that the therapist should “use any of your favorite myofascial, deep tissues, or assisted-stretching techniques to bring length to the front line” and this is correct suggestion but the therapists also need some guidelines.
Let’s address here the techniques which are recommended in the article to work on scoliosis. There are two major components mentioned:
1. The patient’s body is lifted by the therapist while the patient is seated: “the therapist uses one arm to grasp and lift the client’s torso (the client is sitting at this point by JMS), and the other palm to gently spring the vertebrae above and below the rigid hump.”
Yes, this technique is part of the treatment protocol for scoliosis, but it is a very small part and it can be used only at the end of the session. The main part of the session must be done with the patient on the table – first on the stomach with pillows to unload pressure, than on the convex side of the main curvature again with compensatory pillows and finally on the back with pillows under the knees. These positions are a critical part of the treatment because they allow the therapist to work on the paravertebral muscles in the state of maximum relaxation. If even a relaxed patient sits, the paravertebral and quadratus lumborum muscles are still under the basic tension and this fact dramatically decreases the therapist’s chances to recover some balance between both sides.
Let us enumerate the major steps of MEDICAL MASSAGE PROTOCOL in addressing Scoliosis presented in Fig. 2:
1. Relaxation of the paravertebral muscles in areas A and D and stimulation of paravertebral muscles in the areas B and E
2. Decrease tension in intercostal muscles on the left and stimulate them on the right
3. Decrease tension in area C and stimulate muscles in area F
4. Decrease pressure inside the curvature using the left scapula as leverage
5. Decompression of thoracic curvature by compression of the right thoracic cage
6. Traction of the vertebral column
7. Mobilization of the thoracic curvature while the patient is on the left side
8. Work on the abdominal muscles
9. Mobilization of the thoracic curvature using breast bone
10. Mobilization of the lumbar curvature using pelvis and lower extremities
Only at the end of these steps can the patient be seated and the therapist can use the technique described in the article. Thus by itself the mentioned technique doesn’t have even remotely enough clinical power to unload pressure built up in both curvatures.
2. “Begin myofascial work using extended fingers or forearm to hook and scoop the lumbar and/or thoracic erectors up onto scoliotic convexity. Next, dig extended fingers into lamina groove on the concave side and push shortened (guy wire) erectors away from the spine”
The article is completely correct when it suggests using relaxation of the paravertebral muscles inside curvature (areas A and D) by pushing the paravertebral muscles away from the spine.
Now let’s look at treatment recommendations for the erectors outside of the curvature (areas B and E). Image 6 in the article illustrates how to hook and scoop lumbar and thoracic erectors and it is almost the identical application with erectors pushed away from the spine. From reading this article one may only see the difference between convex and concave sides’ applications as the degree of applied pressure.
In clinical reality, relaxation of the paravertebral muscles when it is applied on the convex (outside of the curvature: areas B and E) is completely counter-productive. Instead of decreasing pressure inside of the curvature, such therapy will increase deformation by additionally weakening erectors in the areas B and E. Instead of pushing erectors away from the spine in these areas the therapist must use stimulating techniques: percussion, interruptive vibration, etc., to elicit more tension from the weakened erectors which will be able to provide additional counter-resistance to the further increase of curvature.


Working With Lumbars, Part 2. Massage&Bodywork Magazine, Nov/Dec: 100-101, 2014
By Til Luchau
This article is about treatment of Lumbars and the two techniques mentioned are correct despite that the article gives them incorrect meaning. What we especially don’t like is the author’s manipulation of respected medical sources, his constant ‘borrowings’ of long existing manual techniques and rebranding them as his ‘new’ treatment approaches. Here is quote from the article:
“Back pain linked to the iliolumbar ligaments (ILL) will often be felt by the client as a deep, dull, generalized ache, or sometimes as deep, sharp, sudden pain with spinal rotation or flexion. ILL pain can also refer to the hips, groin, rectum or genitals.”
According to the author he took this information form Travel and Simmons Trigger Point Manual and he provided appropriate reference.
Since this is a completely incorrect statement we went to the same publication and examined every page where Dr. Travel and Dr. Simmons even mentioned the iliolumbar ligament. We can guarantee our readers that there is no information in the textbook which supports the author’s claims.
In the article the author constantly mentioned iliolumbar ligament as if it were an independently acting anatomical structure. According to his article the pain originates in the ligament itself and travels to distant areas. Yes, there is such a thing as Iliolumbar Syndrome which is an inflammation at the iliolumbar ligament insertion into the iliac crest rather than its actual strain. Strain to this ligament is an extremely rare pathology and occurs mostly in athletes, during severe accidents, complicated pregnancies and during childbirth.
Let us give the readers some sense of the issue. In PubMed, which is a worldwide constantly updated collection of medical articles, the entry Iliolumbar Syndrome gives you 11 related sources while entry Sacroiliitis, for example, gives the reader 1505 medical sources.
What is even more surprising is the fact that it seems the author didn’t even bother to look in the Trigger Point Manual which he quoted before writing this article. If he had, he may have found a lot of helpful information which could be shared with therapists. First of all, according to Dr. Travel and Dr. Simmons:
“The iliolumbar ligament develops from immature fibers of the quadratus lumborum muscle…”
Thus the iliolumbar ligament always works in conjunction with the quadratus lumborum muscle, supporting its stabilization efforts at the very end of the rotation and flexion. This is why for the iliolumbar ligament to be injured, the quadratus lumborum muscle must be strained first. It never works the opposite way since deeply located ligaments always fail after more superficially located soft tissue structures give up.
The patient’s position shown in the article for the application of the so called Iliolumbar Technique doesn’t have anything to do with treatment of the iliolumbar ligament. The author took a widely known medical massage technique (see the article which we reviewed above: Freeing the Quadratus Lumborum. Massage&Bodywork Magazine, Nov/Dec: 82-87, 2014
By Peggy Lamb) to address the insertion of the quadratus lumborum muscle into the iliac crest and as he frequently does, conveniently renamed it as the Iliolumbar Technique and now promotes it as his own development.
If the author had carefully read the Trigger Point Manual as well as anatomy textbooks, he would have found that the anterior band of the iliolumbar ligament is completely inaccessible to manual treatment. The posterior band can be reached in skinny patients from the back (not from the side as is presented in the article). Here is quote from Naeim et al., (1982):
“There is also an exquisitely tender point at the posterior (bold by JMS) iliac crest”
This posteriorly located spot is used to inject lidocaine or prolotherapy to the iliolumbar ligament treating Iliolumbar Syndrome. Thus, physicians since the 1980s reach the iliolumbar ligament from the back while Mr. Luchau somehow reaches it from the side. So, someone is wrong and we suspect that it is the author of the article.
For the therapist to ease access to the iliolumbar ligament, two pillows should be placed under the belly. It will ‘bring’ the place of the ligament’s insertion up.
In regard to the statement made in the article that pain from the iliolumbar ligament will travel to the rectum, groin or genitals. This is the author’s pure invention which greatly mislead therapists. Let’s read a medical source which gives the detailed overview of the Iliolumbar Syndrome (Naeim et al., 1982):
“This syndrome has been described as a distinct low back pain syndrome with typical unilateral findings… Many patients complain of ache that is aggravated by prolonged sitting and standing.”
Did readers find in this description the deep, sharp, sudden pain which may radiate to the groin and genitals the author mentioned in the article?
So many times we have caught the author on manipulating medical sources for his own benefits and against the therapists that it is simply sad that this unfortunate trend continues.
REFERENCES
Naeim F, Froetscher L, Hirschberg GG. Treatment of chronic iliolumbar syndrome by infiltration of the iliolumbar ligament. West J Med. 1982 Apr;136(4):372-4.
Travel J.G., Simmons D.G. Myofascial Pain and Dysfunction. Trigger Point Manual. Williams & Wilkins, Baltimore, 1983
MASSAGE TODAY





Creating Better Performance: Investigating Dysfunction. Massage Today, October, 2014, Vol. 14, Issue 10
By Debbie Roberts, LMT
Great article! There is nothing to add. The author exhibited great clinical skills in evaluation and treatment options.



Pediatric Massage: Approach for Congenital Muscular Torticollis. Massage Today, October, 2014, Vol. 14, Issue 10
By Tina Allen, LMT, CPMMT, CPMT, CIMT
This article is about Torticollis and it provides an informative overview of the topic which will definitely help the therapist to understand the nature of this pathology.
However, the treatment part the article completely loses its practical value since it doesn’t give therapists any clinically valuable information and additionally misguides them. The author mentions only three practical recommendations for the treatment of Torticollis by massage therapy:
1. “…gentle stroking techniques to the lateral, posterior and anterior areas of the unaffected side prior to addressing the affected side”
2. “…we do not recommend an involved stretching protocol with children”
3. “…engage the child to turn their head from side to side, bring their head to chest and orient to midline”
The question is why the therapist even needed for such therapy? All of that can be done by parents trained in a day. On the other side, massage therapy is a key treatment option for Torticollis but only when it is done right.
Overall the treatment part of this article reflects a much broader problem with clinical application of Pediatric Massage in the USA. In a majority of cases, articles on this subject have nothing to do with the clinical value of massage for children with various pathologies. Pediatric Massage is for children who really need help and will get great benefits from correctly formulated protocols, not a toothless application of gentle strokes which need to be done by parents rather than a highly trained therapist.
Here is one example from the article:
“…we do not recommend an involved stretching protocol with children.”
Where did this come from? For the entire world, stretching is a part of Torticollis’ treatment but the author, who is considered to be an expert on the subject, does not recommend it in a national professional publication!
We will not cite European medical sources on this subject since we’ve noticed that foreign medical publications for some reason are not considered an authority for many massage educators and American massage professional organizations. Let’s look at what pediatricians here in the USA think about stretching for the Torticollis.
Here is an excerpt from a study on this subject published in Annals of Otology Rhinology and Laryngology by Thomsen and Koltai (1989):
“…these patients (with torticollis by JMS) were managed conservatively with massage and controlled stretching of the neck (bold by JMS). Resolution of the neck mass, the torticollis, and the facial asymmetry occurred in all patients.”
Here is excerpt from an article by Porter and Blount which reviewed several studies around the world on the same subject and was published in American Family Physician (1995):
“Heat, massage and passive stretching exercises (bold by JMS) are the preferred initial treatments for pseudotumor and torticollis. More than 70 percent of patients will respond to this approach.”
Thus, American physicians conducted clinical studies and recommended the use of stretching as an important clinical tool for patients with Torticollis, while the author didn’t recommend it to practitioners to use without even basic explanations why. The practitioners will follow this completely incorrect recommendation and it will be bad for the patients and for the profession.
From massage articles to professional gatherings we continue to hear cries from educators and therapists that American medicine doesn’t recognize massage therapy as an important clinical tool and we need to have more studies to prove massage value. Modern American medicine will never recognize massage therapy if it continues to live within its own system of incorrect beliefs and unscientific assumptions. If you can’t deliver clinical results quickly and efficiently, nobody will listen to you. This is exactly what will happen if therapists use recommendations from this article as a clinical guide for the treatment of Torticollis.
REFERENCES
Porter SB, Blount BW. Pseudotumor of infancy and congenital muscular torticollis. Am Fam Physician. 1995 Nov 1;52(6):1731-6. Review.
Thomsen JR, Koltai PJ. Sternomastoid tumor of infancy. Ann Otol Rhinol Laryngol. 1989 Dec;98(12 Pt 1):955-9.



The Transformation of the TMJ Imbalance. Massage Today, October, 2014, Vol. 14, Issue 10
By Don McCann, MA, LMT, LMHC, CSETT
We may disagree with the author on some theoretical aspects of this article, but overall the tools suggested for the treatment of TMJ dysfunction have their merit. They are not the only solution but should be considered while the protocol is formulated.




Little Muscles Can Create Big Pain. Massage Today, November, 2014, Vol. 14, Issue 11
By David Kent, LMT, NCTMB
This is a good article on tension developed in the gluteus minimus muscle. The presented information is correct and illustrations definitely help.
There is one critical point the author always misses in his article and as a result practitioners make the same mistakes in the therapy room. The author always presents muscle pathologies as local abnormalities. However, in last 10-15 years this local only origin theory has lost its appeal for scientists in somatic medicine because more and more authors have emphasized the importance of the low grade irritation of spinal and peripheral nerves as a main cause of hypertonic muscle pathologies.
Dr. L. Quintner (1994) revived the original theory of the neurological origin of trigger points in muscles proposed by authors of the trigger point concept, Dr. Shade in Germany and Dr. MacKenzie in Great Britain in the 1920es. This new, old concept has great support in the medical community since the local-only approach to treatment proposed by Dr. Travel and Dr. Simmons didn’t provide stable clinical results in all cases of active trigger points.
To summarize. The information in the article is correct and the therapists may use these treatment recommendations only if tension in the gluteus minimus is a result of trauma or overused tension. However if tension in the gluteus minimus developed as a result of irritation of the spinal nerves by:
Tension in the lumbar erectors,
Tension in the quadratus lumborum muscles
Tension in the lumbar rotators
Misalignment of the sacro-iliac joint
Tension in the piriformis muscle,
the local treatment proposed in the article is a waste of time since the real cause is a completely different pathology. It requires the application of a completely different MEDICAL MASSAGE PROTOCOL to address the real cause of tension in the gluteus minimus. Therapists don’t have the professional right to jump to the local treatment option discussed in the article before ruling out pathologies discussed above with the application of simple but informative tests. Otherwise therapists will mislead themselves and their patients.
REFERENCES
Quintner JL, Cohen ML. Referred pain of peripheral nerve origin: an alternative to the “myofascial pain” construct. Clin J Pain. 1994 Sep;10(3):243-51. Review.





Attempting to Explain What Causes Elevated Tissue Density. Massage Today, November, 2014, Vol. 14, Issue 11
By Linda LePelley, RN, NMT
In the April, 2012 issue of Massage Today the author published an article about what she called “Elevated Tissue Density. In this article she proclaimed that tension developed in the soft tissues is the result of an accumulation of cholesterol. This outrageously incorrect statement unfortunately found its way into the pages of a national publication. For almost three years we’ve reviewed every LePelley article and used scientific data and medical sources to inform practitioners about the author’s unscientific claims.
We think we deserve a lot of credit for finally stopping this nonsense. In this issue of Massage Today the author officially dropped her claims about cholesterol’s accumulation, which is good for Massage Today since it will stop promoting unscientific claims on a national stage:
“Having no investigative resources apart from clinical experiences and my own two hands, I resolved to refrain from further open speculation about the cause of elevated TD (bold by JMS) and just focus on sharing my observations and treatment results.”
Great! No more weird theories and we can openly discuss the topic of Tissue Density Restoration Massage developed by the author. We were so excited until we got to the end of the same article, which to our great surprise is titled ‘Hypothesis of the Cause.’
Wait a minute! Just several paragraphs above the author swore to stay away from “…further open speculations about the cause of elevated TD” and now again she is proposing her own “new theory’ of tension developed in the soft tissues. This time it is proteins which are the main cause of soft tissues adhesions:
“It seems plausible to me that the source of invisible chronic pain and elevated TD (tissue density by JMS) is the product of autonomously formed adhesions – strong protein bonds, composed of our own bodies’ natural ingredients due to thermal and/or chemical reactions to environmental circumstances including injuries, overuse, repetitive movement, stress and any other source of inflammation.”
Ironically, the author is now a little bit closer to the truth. When we reviewed Mrs. LePelley articles before, we several times mentioned that according to medical sources the elevated tissue density which the author only recently discovered for herself is a well-known medical phenomenon. It was extensively studied by scientists around the world without knowing that the author would develop her own theories on this matter.
Several times (the readers may find our reviews in Good Apples/Bad Apples section of JMS in 2012) we mentioned that the substances which are initially responsible for tissue tension are called glycoproteins and they are combinations of protein and sugar. The author decided to drop the sugar part from the picture and mentioned only proteins and some mysterious “…our own bodies’ natural ingredients…”.
This question is for Mrs. LePelley: “What natural ingredients are you talking about? Name them and if you can’t you don’t have the right to make your own assumptions which have nothing to do with medical science, especially if you promised to stay away “…from further open speculations”. If these ingredients in fact are carbohydrates as we informed you and readers, we all should celebrate this final moment of clarity for the Tissue Density Restoration Method!”
This question is for Massage Today: “Colleagues, we are in the 21st Century and therapists deserve at least some respect as your readers. How can you publish claims like this one and consider yourself a respected professional publication?”





Is It Time to Reconsider Cryotherapy? Massage Today, November, 2014, Vol. 14, Issue 11
By Whitney Lowe, LMT
The article deserves 10 times more Good Apples. Finally, the voice of reason. For almost 20 years we have emphasized that ice application is a counterproductive treatment option except in cases of acute trauma (first 24 h), acute inflammation (e.g., rheumatoid arthritis) and severe nerve pain (neuralgia). In all other cases ice kills the therapist’s work. We are glad that now we are not alone.

The Aspiration to Prevent Hip, Knee and Shoulder Replacements. Massage Today, November, 2014, Vol. 14, Issue 11
By Dale G. Alexander, LMT, MA, PhD
First of all, this article has important practical potential. We completely agree with the author who emphasizes the importance of early screening for degenerative changes in the major joints:
“The important question is whether each of us has the skill sets to screen for early indicators that these joints may be progressing toward degeneration.”
The article gives some basic tips for such screening, which is helpful. What is always fascinating about Mr. Alexander’s articles is his own absolutely weird theories which he tries to spread among practitioners. This article is no exception. Mr. Alexander again enlightens us all on human developmental history in the form of our primal ancestors falling from the trees at alarming rates and the genetic impact of these countless falls at the dawn of humanity on the formation of our shoulder, hip and knee joints.
“I further propose that the degeneration of the hip, knee and shoulder may have an evolutionary linkage. My conjecture is that their inherent weaknesses come to us as an evolutionary predisposition from our time as primates living in trees. A fall from a height all too often led to an immediate or eventually related death. Those dead primates’ genes were not passed on. As a result, I propose that nature selected for a more flexible anterior shoulder capsule and a more distensible posterior hip capsule to assist the capacity to “tuck and roll” during a sudden fall.”
If the author ever visited a local zoo he might see that monkeys never fall from trees except when they are sick or fight with each other. This is exactly why our ancestors lived in trees – to avoid danger and according to basic biology, they survived because they were so good. Of course from the author’s point of view, it is very dangerous to climb and live in trees, but the author maybe doesn’t realize that his ancestors simply lost those skills long ago.
To carry the author’s ‘profound’ thinking process further, if his little theoretical gem is correct it becomes obvious that our ancestors got down from the trees and became humans just because they were tired of constantly falling from the height and decided to walk on two just to avoid horrible death or constant bouncing off the ground. This is simply a ‘new’ dawn in evolutionary science.
In reality the formation of the major joints which the author tirelessly tries to explain in his ‘work,’ which can be published only on the pages of Massage Today, is the result of the gradual abandoning of walking on four by our ancestors and the appearance on the evolutionary scale of so called Homo Erectus, who started to walk on two. That was what formed our major joints.
Thus, falling from trees at such an alarming rate that it changed the anatomical structures of our ancestors’ major joints is the result of the author’s wild personal imagination. Unfortunately, Massage Today allows these sad articles to be published and re-published nationally.

Using Your Intuition in the Decision Making Process. Massage Today, November, 2014, Vol. 14, Issue 11
By Marie-Christine Lochot, LMT
This article is about intuition and its role in the decision making process. The article addresses an important topic which is very helpful in the clinical application of massage. The author quoted Albert Einstein and other scientists on the value of intuition and she is absolutely correct since intuition has played a major role in many world discoveries.
However, we think the author didn’t fully understand the topic she was writing about. Here is a quote which summarizes the author’s views:
“As we talk with clients, let’s pay attention to our body reactions, to our guts, to the sounds around us and anything unusual.”
The article misses the point of intuition as a concept. Einstein didn’t talk about sounds around us or our bodily reactions. He and others quoted in the article were talking about intuition based on a profound knowledge of the topic. In such cases the scientist or therapist constantly thinks about solving the problem or dealing with a difficult patient and suddenly they come up with a solution. This moment of clarity is the result of their brain continuing to work on the problem even when they are asleep (e.g., the periodic table came to Mendeleev during his sleep and it created modern chemistry). Thus, intuition is a result of knowledge and accumulated clinical experiences rather than unusual sounds, smells, lights or body reactions.



Learning a Hands-Free Solution to Fix SI Dysfunction. Massage Today, November, 2014, Vol. 14, Issue 12
By Debbie Roberts, LMT
This article is about sacroiliac joint dysfunction and how to help patients without any type of bodywork using sets of exercise, breathing exercise etc.
Overall this a good article which provides very helpful recommendations the therapist should consider. However, we have same problem with this article as with many other published in national publications. This problem is fragmentation of the profession.
SI joint dysfunction is a very complex problem and its treatment is challenging especially in older patients when SI joints greatly reduce their mobility. The information in the article is correct as part of the integrative approach to the rehabilitation of all patients with SI joint dysfunction. The information in the article is presented as a solution to the problem, while in the real life it is only part of the solution which must also involve other modalities and protocols combined for the patients’ benefits.

Using Massage to Address Pediatric Digestive Issues. Massage Today, November, 2014, Vol. 14, Issue 12
By Tina Allen, LMT, CPMMT, CPMT, CIMT
The article generally outlines the need for abdominal massage for children suffering from constipation. The author is correct when she points out the vital role of abdominal massage in the management of constipation.
The treatment recommendations are very basic. If the author proclaims that abdominal massage must be “…led by a Certified Pediatric Massage Therapist” than it is really puzzling why two such basic things as “…circular strokes on the abdominal area, they should always follow the direction of the child’s digestive tract” and “… not put any pressure on the Xyphoid process” require a certified therapist since parents can and should be easily taught in one hour to do exactly the same thing.
Let’s look at the very basics. According to Wikipedia: “Pediatrics is the branch of medicine that deals with the medical care of infants, children, and adolescents, and the age limit usually ranges from birth up to 18.”
This and a previous article confused Baby Massage, which is an important tool for the baby’s development, with Pediatric Massage, which is supposed to deal with “…medical care of infants, children and adolescents.” The relation between Baby Massage and Pediatric Massage is exactly the same as between Swedish Massage and Medical Massage.
MASSAGE MAGAZINE




Topical Analgesics & Massage. Massage Magazine, Issue 222, Nov: 20-22, 2014
By Michael McGillicuddy LMT, NCTMB, Lynda Solien-Wolfe, LMT, NCTMB
An informative article about topical analgesics and the basic principles of their application. It will be helpful to practitioners who would like to use it as an additional modality to speed up client’s recovery.


Neural Reset Therapy. Massage Magazine, Issue 222, Nov: 58-62, 2014
By Lawrence Woods, LMT
This article introduces Neural Reset Therapy developed by the author. This is a great example of massage therapy living in its own bubble. The author successfully invented a modality which has been used for decades by osteopathic physicians and physical therapists around the world.
However, as a matter of clinical value, the information in the article is correct in many aspects but misses a lot of very important information.
Yes, the article is correct when it emphasizes the value of engaging the central and peripheral nervous systems as critical components of clinically sound massage therapy. The correct level, anatomical location and way the peripheral sensory receptors are activated are very important components of the therapy since it engages the patient’s nervous system in the treatment. Also, treatment on the ipsilateral to the spastic area side is another correctly mentioned approach. The article claims that Neural Reset Therapy addresses all of that. Since there is no actual description of the treatment procedure (pictures are uninformative) it is impossible to evaluate its effectiveness.
Let’s believe that NRS is as effective as the article proclaims. In such case there are some questions remaining unanswered. For example, a quote from the article:
“…it would only take you at most 20 or 30 seconds – or as little as three seconds – to effect a major change even in troublesome muscles like the upper trapezius or hamstrings. Imagine the surprise on your client’s face if you could eliminate all of the muscular pain in her neck in three to five minutes.”
That is it: no more and no less, but all problems somatic medicine continues to face once and for all are solved thanks to NRT! Nothing in Medical Massage and manual therapy gives the therapist and patient the luxury of healing in 3-5 minutes. The author must be careful with statements like this one if he wants serious therapists even look at NRT.
Is there a chance that 3, 20 or 30 seconds of therapy can reduce muscle tension? Yes, activation of H-reflex will do that Goldberg et al., (1992). However, this is a very short lived effect since the tension will come back quickly. This is why such therapies as activation of H-reflex are used in somatic medicine as a supportive introduction to more sophisticated approaches, e.g., resetting muscle spindle receptors.
It is mistake to take valuable components of somatic rehabilitation which are normally applied only in conjunction with other modalities and make them individually applied techniques. At the end of the article the author recommends using NRT as a component of the treatment session and that makes more sense.
REFERENCES
Goldberg, Joanne; Sullivan, Seaborne (1992). Effect of Two Intensities of Massage on H-reflex amplitude. Journal of the American Physical Therapy Association 72: 449–457.
MASSAGE THERAPY JOURNAL





Stretching and Strengthening the Spinal Curves. MTJ, 53(4): 21-28, 2014
By Joseph E. Muscolino
A very good and informative article with great illustrations.




Massage+Medications. MTJ, 53(4): 36-44, 2014
By Helen Tosch
This article outlines various groups of medications, their side effects and correlations with massage therapy sessions.





Massage & Anterior Hip Replacement. MTJ, 53(4): 46-51, 2014
By Elizabeth McIntyre, MAS, BSN, RN, LMT
A very good overview of hip replacement using an anterior approach. The massage therapist’s involvement before and after surgery is correctly outlined.



 (subject)
(subject)



 (content)
(content)
Introduction to Sports Massage Therapy. MTJ, 53(4): 46-51, 2014
By Steve Jurch
This is a very weird rating but it reflects the nature of the article. The real subject of this piece is Clinical Massage rather than Sports Massage as it claims in its title. The author exhibits a very good knowledge of clinical massage’s application for clients who develop injuries as a result of various sports. In JMS we’ve had several articles on this subject.
We posed readers to answer a very simple question: “What is the difference between the client who pulls an Achilles tendon during a sporting event and the client who pulls the same tendon by slipping on the floor in the supermarket? They are absolutely identical injuries but the therapist who works on the client with a strained tendon as a result of slipping on the floor will never advertise himself as a Supermarket Massage Therapist! Thus, the place where the injury occurred or a specific population don’t constitute the type of massage therapy. However, the article mistakenly proclaims that:
“The same techniques that are utilized in other types of massage are used in sports massage, but are applied to a specific population.”
This is a complete misunderstanding of the scientific concept of Sports Massage. Yes, the techniques are the same but their goals, speed, combinations and sequences are completely different from Swedish Massage or Medical Massage.
In such case what constitutes Sports Massage? Unfortunately the real topic of Sports Massage wasn’t even covered in the article. Sports Massage is applied on healthy athletes or sports enthusiasts as a preventive measure to avoid injuries. This is exactly what Paavo Nurmi, who was mentioned in the article, received during the Olympic Games in Paris in 1924. As soon as an injury occurs the client is under the technical umbrella of Medical Massage. Thus the real Sports Massage is completely different from what is described in the article where the author didn’t even mention pre-event, post-event, rehabilitative massage etc., which are part of Sports Massage Science.
The massage therapists who work with athletes and sports enthusiasts must have a basic understanding of the topic and easily switch from Sports Massage to Medical Massage and vice versa depending on the client’s needs.
Since there is no actual Sports Massage as a preventive measure in the article, its title should be “An Introduction to Medical Massage Therapy in Cases of Acute Injuries” and this would be a very good piece. Overall the article robs therapists of the real value and meaning of Sports Massage.
For more information on Sports Massage Science, please read articles on this subject in #5, 2009, #1, 2014 JMS.
Category: Good Apples, Bad Apples
Tags: Issue #1 2015