PART III: MANUAL LYMPH DRAINAGE PROTOCOL
John F. Mramor, MA, LMT, CLT, NCTMB, CR, RM
Medical Advisors:
Michael Harrington, MD, Director, Palliative Care Consult Service, MetroHealth Medical Center and Assistant Professor, Case Western Reserve University School of Medicine
Walter George, MD, Medical Director, Crossroads Hospice, Cleveland, Ohio
This is the final part of our article on Ascites and its treatment by Manual Lymph Drainage (MLD). In Part I (see Issue #1, JMS, 2015) we discussed the pathology of Ascites and its modern management by different medical procedures. Part II (see Issue #2, JMS, 2015 ) covered theoretical aspects of MLD application and in this final part we cover basic MLD protocol.
There are no two identical patients with Ascites since always there will be clinical variations. This article will not cover all clinical situations but presents the basic protocol which should be altered if needed to adapt to the patient’s needs. Thus this is the treatment plan for a “normal” case of Ascites, regardless of whether cirrhotic or malignant.
Of the four strokes utilized in MLD, only two are utilized in the management of Ascites: stationary circles and pump. Finger-tip effleurage and fascial stretching are used on a limited basis. Deep diaphragmatic breathing during a session is helpful, but for some patients, this is not possible. Abdominal girth measurements are performed each Monday prior to the session and every Friday after the session. Weights may also be taken in the same manner.
During the therapy the patient should be supine. Most will not be comfortable lying flat, so an angled position is fine. The patient should be entirely disrobed from the waist up. If pants are not removed, then at least have the patient draw them downwards so that the therapist can easily manipulate the pelvic/pubic regions. Women are to have a towel draped across the breasts, making sure that the towel is not so large that the therapist cannot access the lateral ribcage without need to constantly move the towel about.
If it’s possible, ask the patient about long exhalations to fit 3-4 strokes into one exhalation. If the patient has breathing difficulties, the therapist should use the same protocol but do strokes with a slower pace. Here is the protocol of MLD for Ascites that we use in our clinic. Please be aware that in cases of severe Ascites the application of the strokes suggested in the videos must be slowed by 50%.
Step 1. With stationary circles, stimulate the cervical lymph nodes, the supraclavicular nodes and finally the anterior and posterior shoulder. The video below shows the application of stationary circles in each area except the posterior shoulder.
Step 2. Using finger-tip effleurage, stimulate the inter-axillary anastomoses. Perform this with both hands simultaneously sliding from the sternum moving laterally towards the axilla. Repeat 7 to 10 times.
Step 3. Stimulate the axillary lymph nodes on the inner arm and in the axillary fold, 5 to 7 times with stationary circles.
Step 4. Open the anterior inter-inguinal axillary anastomoses (AIIA), bilaterally, using Vodder’s procedure.
a. Perform stationary circles above the horizontal watershed.
The video below illustrates the application of strokes.
b. Perform stationary circles below the horizontal watershed to route or mobilize fluid proximally all the way to the axilla itself, completing 5 to 7 routes. The video below illustrates this segment of the therapy.
c. Route fluid 5-7 times from the inguinal region to the axilla and add application of pumping strokes at the end of stationary circles when they stop just below the axilla. This is a final sequence of opening the Anterior Vertical Watershed (see Fig. 1).
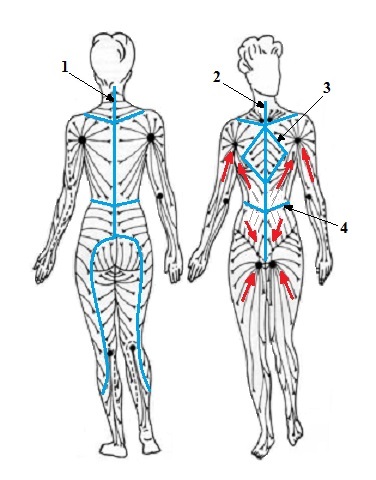
Fig. 1. Normal lymph drainage and watersheds (blue lines)
1 – posterior vertical watershed
2 – anterior vertical watershed
3 – thoracic watershed
4 – transverse watershed
Red arrows – direction of lymph drainage to axillary and inguinal lymph nodes
Step 5. Re-work the axillary lymph nodes, 3 to 5 times (repeat Step 3).
Step 6. Re-work the AIIA with 7 to 15 passes, bilaterally, twice.
From mid-line moving laterally to the AIIA, adjacent to the umbilicus and proximally to the xyphoid process, mobilize fluid using stationary circles, sweeping this region with 7 to 15 passes. Same as Step 4 ‘c’ or Video #6 but stationary strokes.
Step 7. Repeat #6.
Step 8. Repeat #7.
Step 9. Stimulate the inguinal lymph nodes with stationary circles and pumping strokes (see video below).
Step 10. Have the patient perform deep diaphragmatic respirations to tolerance.
Step 11. Repeat Step 3.
Step 12. Repeat Step 6.
Step 13. Repeat Step 9.
Step 14. Repeat Step 10.
Step 15. Perform a fascial stretch along the Anterior Vertical Watershed (see Fig. 1), simultaneously bilaterally, in two sets (in order to cover the entire length of the route). To do that correctly, place both hands on the lateral sides – one on the left and one on the right – about in line with the umbilicus and stretch the skin slowly in the opposite direction. Increase the range of the stretch slowly over a period of several seconds. For the next part, place hands higher so they are almost on the level of the axillae, stretching the skin once again over a period of several seconds.
Step 16. Repeat Step 3.
Step 17. Repeat Step 2.
Step 18. Repeat Step 1.
The entire procedure typically takes one solid hour. The author has found that most patients find it quite comforting and usually enter a sleep state during the process. Some have even experienced altered states due to the hypnotic-like rhythm of the hands or use it as a mechanism through which meditative prayer is accessed.
This procedure is repeated daily, Monday through Friday. It is best to schedule sessions either prior to breakfast, prior to lunch or prior to dinner. If the case is severe (near or over 200 cm girth), Saturday treatments may be necessary or twice daily sessions for a few weeks until measurements prove satisfactory. Sessions are continued for the duration of the patient’s stay in hospice, obviously ceasing once signs/symptoms of serious decline are evident. It is possible to titrate frequently, especially given the intensity of daily treatments. The author recommends doing this after at least three to six weeks of daily sessions. Less than three sessions per week is meaningless and it may be necessary to increase the frequency of intervals thereafter.
Remember, the goal is not to seek a continual decrease in abdominal measurements from week to week. Ascites will accumulate regardless of any palliative treatment intervention. The best case scenario is stabilizing measures or slightly lowering them from Monday to Friday. Do not be disappointed if the weekend hiatus yields more fluid. This is unavoidable. The goal is to delay or slow the re-accumulation of fluid over time.
CONCLUSION
To practice the art of Manual Lymph Drainage within a population so fragile is a blessing not only to the patient, but a privilege to the therapist. These patients are suffering in a variety of ways, most likely placed in hospice or palliative care and facing the end of their lives. To offer them an intervention that is simultaneously addressing Ascites, providing solace and nurturing their grieving hearts is not something to be flippantly dismissed. Often, usually due to the multidimensional approach that therapists will provide, patients will blossom in one or several ways, thus impacting their quality of life. Unfortunately all patients eventually die, but because of the power inherent in the technique and the focus on serving with a heart that encapsulates the totality of patients’ life experiences, not just their bodies but their lives are invariably enhanced.
Further research is necessary to validate and enhance the application of the MLD technique for Ascites patients and the author wholeheartedly calls thescientific community to do that. For now, though,allow this to be one more tool in the arsenal to assist people suffering from this debilitating symptom. This tool has few side effects, can improve a patient’s life in many ways and is of low cost. It is time to consider touch.
Category: Medical Massage
