JMS and our readers were very fortunate when Dr. J. Sharkey contributed his first article on Biotensegrity in 2015 (https://www.scienceofmassage.com/2015/11/concept-of-biotensegrity/ ). We consider his and his colleagues work as a great contribution to the theory and application of clinical massage therapy in general and Medical Massage in particular.
In the last issue, Dr. Sharkey gave an interview to JMS in the Person of the Month section ( https://www.scienceofmassage.com/2019/06/person-of-the-month-issue-2-2019/ ) and now we are gladly publishing his second article on the subject.
It doesn’t matter how many textbooks a therapist reads, or videos seen or how many body’s plastic models and diagrams he or she examines. There is no substitute to live dissection course when complex interactions between tissues and organs can be observed directly.
There are a limited number of dissection courses offered to therapists and even within this niche we highly recommend our readers consider Dr. Sharkey’s internationally acclaimed courses. The critical difference is that he conducts classes from the therapist’s clinical perspective rather than pure anatomical study. Therapists may learn more about Dr. Sharkey’s dissection classes here: https://www.ntc.ie/dissection-usa/
Dr. Ross Turchaninov, Editor in Chief
BIOTENSEGRITY – ANATOMY FOR THE 21ST CENTURY
Thoughts On Fluid Dynamics And Biotensegrity
By John Sharkey, Clinical Anatomist, Ireland
email: john.sharkey@ntc.ie
“This philosophy has chosen the fascia as a foundation on which we stand … By its action we live and by its failure we die … The soul of man with all the streams of pure living water seems to dwell in the fascia of his body.”
– Dr. A. T. Still
INTRODUCTION
Biotensegrity is a model that provides a rich tapestry of the architecture of our living, breathing body seeing as whole in all its complexity. On the other side, fascia is the fabric which unites the human body in perfectly arranged form and therefore Biotensegrity and fascia are two intrinsically coupled concepts. The term ‘Biotensegrity’ is an extension of Fuller’s term “tensegrity, a syntactic of “tension” and “integrity” which is applied to living tissues and that gave word prefix – ‘bio.’
I will address the Concept of Biotensegrity and some other issues in this article. Medical Massage Therapists should integrate the concept of Biotensegrity-Anatomy for the 21st century into their clinical practices. Understanding Biotensegrity has wide reaching implications for Medical Massage therapists and for all other forms of clinical massage. We should finally stop to treat patients using the pure structuralism model which dominated somatic medicine for years. It is time to change these partial views of body arrangement and move to clinical practice based on the modern science.
Also, I would like to discuss fluid dynamics and the significant role it plays in the formation and function of connective tissue, its contribution to the physiological distribution of tension and compression forces within normal homeostasis and also fluid dynamics in pathology.
INNER OCEANS AND BIOTENSEGRITY
To fully understand the anatomy, physiology and morphology of fascia and other connective tissue structures we should consider that our bodies are primarily made of water. The human brain (not including Cerebrospinal Fluid or CSF) is approximately 81% water. Peripheral body fluid stored in muscles and connective tissues can vary between 50 and 75% water while bone has approximately 31%. Thus, the average percentage of water in humans varies according to age and gender and this percentage is significantly higher in babies (75-85%) reducing year by year later in life.
We are, in effect, walking water. I urge therapists to remember that each time you place your hands upon a patient. You are working on a fluid medium! Consider adjusting your treatment strategy according to this very basic concept. Here is a very simple example of such adjustment. Every technique or modality the therapist uses must be finished with appropriate drainage of the tissue. This is the only correct foundation to move forward with therapy.
One of the few places we find free water in the human body is in the urinary system. That said, you can squeeze any human tissue as hard as you like, and no water will emerge. Why? Much of our body’s water is locked up in our intracellular and extracellular fluids including blood plasma, cerebrospinal fluid, lymph and interstitial fluid. This water can only be released through physiology of metabolism since it is bound to collagen. Bound water is very different from the water we drink as it is bound in from colloids inside the tissue and organs and does not swish around our joints or fill up cavities. However, trauma or inflammation may release bound water using various inflammatory substances and the therapist will see it as peripheral edema, for example.
Fluid dynamics is the study of the flow of liquids (and gases), in and around more solid structures. Similarly to rivers shaping the landscape on this blue dot we call Earth, our internal rivers, streams and pools influence the shape and morphology of cells and tissues. Stagnant fluids lead to a change in acidity, abnormal metabolism and the production of pain generating pro-inflammatory cytokines.
How can we, as somatic manual therapists use fluid dynamic to create curative responses and corrective structural changes while working within this water based connective tissue we call fascia? The answer is Biotensegrity informed touch. It means that the Medical Massage therapist first of all should use informed palpation to identify the pattern of tensional pathways which formed as the result of initial somatic abnormalities and detect how far they spread from the area of original pain and dysfunction.
In the Biotensegrity treatment model the Medical Massage therapist must have wider, integrative vision of somatic rehabilitation which allows him or her to re-arrange soft tissues throughout the entire body while restoring normal interactions between them. To do so the removal of initial abnormal stiffness, restoration of normal distribution of tension, will eventually allow restoration of the proper fluid dynamic essential for the physiological functions of soft tissues and body as a whole.
What impact does fluid flow have on tension and compression forces affecting such vital structures such as cell membranes, blood vessels, peripheral nerves, lymphatic or osseofascial structures? It is obvious that unduly stiff, hard and unyielding structures would do little good for living organisms.
Living tissues and organs require short- and longer-term abilities to adapt, alter and vary their basic arrangements due to constantly changing environment and the forces therein (Avison 2015). If bones were rigid unyielding structures, we would experience fractures with every excessive load application. Why didn’t it happen? Because bones are a continuity of our fascial network (see Fig. 1). They also contain water with high levels of hydroxyapatite, i.e., calcium crystals as well as collagen fibers which give bone its elasticity (Sharkey, 2019).
While hydroxyapatite provides the appropriate level of stiffness required to store and release energy when it is necessary for postural support, its combination with collagen transfers and shares forces to more distant tissues via the mechanism of Mechanotransduction (Ingber, 2008; Tomasek et al., 2002; Beloussov, 2006).
Mechanotransduction is the processes through which living cells sense and respond to externally applied mechanical stimuli (e.g., running or massage strokes) by converting them into biochemical signals that elicit specific cellular responses. Without the chain of these events the stiffened fascia would not let us move freely (Sharkey, 2019).
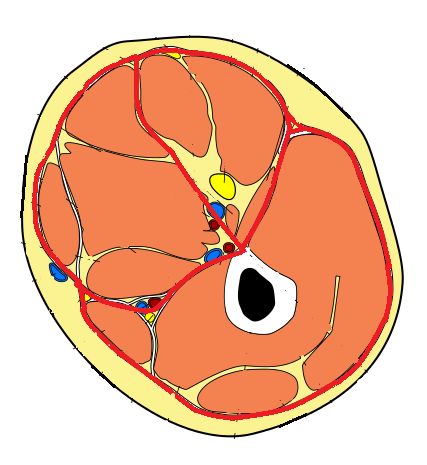
Please carefully examine the image presented in Fig. 1. What you see is a unique image of a plastinated cross-section of the thigh. Plastination is a process which allows anatomists to preserve bodies or body parts. In a fresh cadaver specimen the water and fat are replaced by plastics preserving tissues from the decay while retaining the original properties of the sample. In the original specimen (Fig. 1a) all soft tissues of the thigh were removed except superficial, deep fascia and periosteum which covers the femur. Fig. 1b illustrates diagram of cross-section of the thigh. All tissues between red lines were removed and remaining fascia and femur plastinated as it is shown in Fig. 1a.
ab
Fig. 1. Cross-section of the thigh
a. Plastinated cross section of the thigh which illustrates osseofascial network. Image by Stecco, C., Sharkey, J., Schleip, R. 2018. (fascial Net Plastination Project. FNPP)
b. Diagram of thigh anatomy (red lines are locations of fascia)
Thus after, all soft tissues from the cross-section presented in Fig.1 were removed and only superficial, deep fascia, periosteum, bone and bone marrow remained. These tissues were plastinated to clearly illustrate direct connections and interactions between superficial and deep fascia and periosteum which is a structural component of each bone.
Let’s say that the patient traumatized his biceps femoris muscle and blood leaked between myofibrils and saturated the muscle. Release of unbound water into the tissues immediately increases the muscle’s cross section, and as a result the fascia which covers traumatized muscle becomes overstretched and tight. Besides that, unbound water will saturate fascia itself additionally contributing to its tension.
Eventually this new, pathological tension will spread along the fascia to the lumbodorsal fascia in the lower back, but it will also spread along the deep fascia all the way to its insertion into the periosteum which covers underlying femur. This new tension force will illicit pressure on the periosteum of the femur. Fascia’s attachment to periosteum of the femur is clearly visible on the specimen (see Fig.1). Since the periosteum is a very richly innervated membrane its tension will contribute to the pain intensity, postural changes and gait alternation which additionally amplify the intensity of clinical picture in the posterior thigh. Since tension spreads along fascial planes the same patient will complain about tension and discomfort in the lower back and leg. Thus, initial trauma triggered pathological fluid dynamic which in turn started a chain of events which now affects the thigh as well as far away parts of the body.
I believe that the Biotensegrity Concept is one of the most important developments in medical science, manual therapies and movement therapy in the modern era.
OUR MIRACULOUS CONSTRUCT
Human body is a miraculous construct and we are not defined by the simple fact that we utilize sophisticated bipedal locomotion. Diving beneath the flesh we discover we have thoughts, emotions, consciousness; we have feelings and our body responds to them accordingly.
Historically speaking, anatomical studies have always concentrated on specialties. We focused and studied each system of organs or arrangement of the tissue separately. Thus, everything was done with very precise, but isolated views. Each anatomy textbook presented information in separate sections or chapters by systems or type of the tissues. From generation to generation physicians and therapists around the world were trained that way and it created a correct, but fragmented view of the human anatomy.
In contrast, Biotensegrity promotes a language of “Whole” (an integrative view) while recognizing that a language of “parts” is necessary. When discussing Biotensegrity, classical anatomy provides a foundation upon which we can discuss the isolated organ or tissue, but then place it in the context of the whole.
The language of Biotensegrity is the language of soft matter physics (Levin, 1982). The premise of Biotensegrity is non-linear continuous matter that is self-generated, self-organizing, self-stressing, hierarchical, load distributing and low energy consuming. There are no shear moments, no bending moments, no levers and no joints (Levin. 1981). In other words there are no pin-joints as suggested by classical biomechanics responsible for constructivistic approach to the therapy.
Our bodies are self-constructed and self-governing on the basis of constantly altering and fluctuating tensions and floating compressions. We grow ourselves with tension (mechanical load, receptive muscle contractions, force of gravity, etc). Continuous unmovable compression load, such as is seen in block buildings, would not be a good architectural model for any living structure.
When we look at the tissues under the skin, in a cadaveric specimen, we clearly see that it is not a stratification or layer by layer arrangement of the soft tissues what makes our body such a dynamic, powerful and perfectly adapting structure. I will compare action of living soft tissues during our locomotion to melted lava which roles along the slope with perfect and unstoppable pattern (see Fig. 2). Soft tissue stratification forms when there is a lack of normal tension and mobility which accompanies different pathological conditions. In such case, soft tissue stratification forms the same way as lava cools off.
All living tissues are soft matter and hard matter mechanics (e.g., building and bridges or machinery) cannot substitute for soft matter physics. Thus, we don’t have the right to apply the same rules of structuralism which govern behaviour of non-living structures to the human body in the classroom or in the therapy room.
Fig. 2. Skin and underlying layers of soft tissues (With kind permission from Stecco, C. 2012 personal correspondence).
THE JOINT SPACE AND FOUR BAR (MULTI-BAR) LINKAGE
Let’s do some magic and consider that your skin and soft tissues (muscles, fascia, viscera and all) disappear. What would happen to your skeletal system? It would crash to the floor. But what if magic would remove all your bones, leaving only the soft tissues? Again, we would gather in a soft heap on the floor.
So what is holding us up? In such a scenario it is easy to conclude that it is the relationship between the soft tissues and bones working in continuity giving stability and “lift.” It is this lift that protects the integrity of our joint space.
Our body as a tensegrity structure has both a ‘discontinuous compression’ part and a ‘continuous tensional’ part (Levin. 1982). We should see humans’ skeletal system as the ‘discontinuous component’ and the soft tissues (fascia, ligaments, tendons etc.) as the ‘continuous component.’
Endoscopic live videos recently recorded by my colleague Dr. Guimberteau (2018) reflects Biotensegrity in motion. Visible everywhere are structures that ensure a gliding movement between the aponeuroses, the subcutaneous fat and the dermis. The word gliding is important to discuss here since tissues in the human body rather glide relatively to each other, but they do not slide as therapists frequently think about their dynamic interaction.
In my view the use of the word ‘sliding’ reflects a common misunderstanding in anatomy. Sliding would result in friction and heat generation, but tensegrity structures (when working as designed) are frictionless as seen it even in the joints. The change in the concept of ‘sliding’ to ‘gliding’ also has implications on our view on nature “stretching” used during different therapies. Since tissues glide and morph together with each other, to facilitate movement, the overstretching of the soft tissues may become a problem rather than solution.
The joints in our bodies are not made of overlapping bones with pins at either end to secure their positions accurately in an effort to eliminate transversal shifting forces. Our vertebral bodies do not slide off each other when we bend forwards or sideways, even with a twist. If we have purely mechanistical view on let’s say the elbow joint than we should expect a hole in the distal humerus and a hole in the proximal ulna for bones to overlap and a pin through the holes screwed securely in place. However, the structure of the live elbow is completely different and much more complex and continued than mechanistical view of it.
Joint space and its integrity are maintained through the omnidirectionality of our living tissues, continuous from finger to toe, from side to side, front to back and top to bottom. The body having originated from one cell has developed, grown and rotated back on itself creating the familiar helical basis of all living structures. The Möbius strip concept (see Fig. 3) is evident everywhere in the human body from the anatomy of joints to that of the continuous myofascial and osseofascial tissues (Scar, 2018).
Fig. 3. Möbius strip
The Möbius strip concept moves us from a linear mechanics, hinge like joints and linear muscle contractions mentality to an integrative, continuously tensioned contractile fabric that facilitates our body’s kinematic chain.
It helps to explain, through stored and returned energy in fascia, bone and tendons, how the kangaroo’s tendon does not combust into flames on each hop (Fig 4). It also explains why the Northern Wheatear, a tiny insect-eating Arctic bird, can travel an enormous 9,000-mile return journey every year without cooking itself to death during the migration.
Fig. 4. Biotensegrity explains how kangaroos can jump without burning or cooking their own tendons with each hop.
In addition, it moves us to a new vision of bones (osseofascial system) as primary force generators in movement (Sharkey. 2019 a). Biotensegrity is a force transmission of our energy efficient system. It helps to explain why a person may be hurting in part of the body part (the messenger) while the initial trigger of the pain and discomfort is hiding in a completely different location. Excessive compression or tension can express itself at the weakest point within the Biotensegrity system and this point must be identified by the therapist before treatment starts.
Thus, the model of Biotensegrity has major implications for any manual rehabilitation technique used as a component of Medical Massage such as Positional Release and Strain Counter-Strain, Soft-Tissue Release etc.
In fact, in her recent best-selling book “Yoga Fascia Anatomy and Movement “(Avison. 2015) Avison makes the point “The implications of understanding tensional forces in this context are exceptionally valuable for yoga teaching.” The same can be said for all movement and bodywork models including but not limited to Feldenkrais, Alexander technique, Neuromuscular Therapy, Medical Massage, Osteopaths, Chiropractic, and others.
THE BURNING QUESTION
This brings us to the burning question which is key to Medical Massage practice. How do we translate forces employed in Medical Massage into the Biotensegrity specific resonance that will ensure therapeutic responses at cellular, fluid and tissue level? That cannot occur by chance. It requires expertise in the patient’s evaluation including very skilled palpation training and expertise. Also, it requires advanced understanding of the value and principles of soft tissue manipulation based strictly on modern scientific data to ensure continuous, non-invasive ‘Guided Stress Transfer’.
Such an approach requires that the therapist see even initial contact with the patient’s skin as the ultimate interaction with the deeper cells and tissues. It also requires patience and stillness. Slow, steady and continuous approach to somatic rehabilitation is the order of the day. We also must remember that any physical contact between two bodies (in this case two people) is, in the first place, a portal of stress transfer and energy exchange from one person to another.
There is another aspect of the Biotensegrity Concept within Medical Massage. It is the necessity of the therapist to understand and use correct treatment vectors such as force, intensity, direction, duration, sequencing, velocity and depth of the strokes. Finally, the size of the contact area used during the therapy is also a critical factor since it controls the appropriate level and magnitude of the elicited local pressure in the tissue and using facial planes alters and causes distant tension within the soft tissues the therapist didn’t even touch during the local treatment.
All these events are active components participating in mechanotransduction or stress guided transfer which is a major healing mechanism of soft tissue rehabilitation. In manual therapy it is known as Specific Adaptation to Imposed Demands (SAID). The application of the mechanical force on a targeted tissue translates into a change in spatial and textural properties of the matter and it also impacts body fluids dynamic.
Thanks to scientists like my mentor Dr. David G. Simons, (co-author of the famous big red books “Myofascial Pain, Dysfunction and Myofascial Trigger Points”), we know that the force of gravity acts upon us affecting each aspect of our body functions, shaping it and greatly contributes to so-called pre-stress. Surgeons witness this pre-stress firsthand when living soft tissues retract from the blade every time the surgeon makes an incision.
Until recently countless studies concentrated specifically on the muscles with little attention given to the fascia. Finally, this one-sided approach changed and in a large degree thanks to the modern Biotensegrity Concept which allowed us to see the body’s structural arrangement and functions in its multidimensional complexity.
REFERENCES
Avison, J. 2015. YOGA Fascia, Form and Functional Movement. Handspring Publishing.
Beloussov, L. 2006. Direct physical formation of anatomical structures by cell traction forces. An interview with Albert Harris. International Journal of Developmental Biology 4. 50: 93 – 101
Guimberteau J, Delage J, McGrouther D, Wong J., 2010. The microvacuolar system: how connective tissue sliding works. J Hand Surg Eur. 2010; 35(8):614–622.
Huijing, P. A., 2003. Muscular force transmission necessitates a multilevel integrative approach to the analysis of function of skeletal muscle. Excerc, Sport Sci. Rev. 31, 167-175.
Ingber, D. E. 2008 a. Tensegrity-based mechanosensing from macro to micro. Prog Biophys Mol Biol. 97(2-3):163-179.
Ingber, D. 2008 b. Tensegrity and Mechanotransduction. Journal of Bodywork and Movement Therapies. July: 12(3): 198-200
Levin, S. M., 1981. The icosahedron as a biologic support system; Houston. Alliance for Engineering in Medicine and Biology. p 404.
Levin, S. M., 1982. Continuous tension, discontinuous compression, a model for biomechanical support of the body. Bulletin of Structural Integration, Rolf Institute, Bolder: 31-33.
Levin, S. M., 1995. The Importance of Soft Tissues for Structural Support of the Body. Spine: State of the Art Reviews, Volume 9/Number 2, May
Scarr, G. 2018, 2nd Edition. Biotensegrity: the structural basis of life. Handspring Publishing,Edinburgh.
Sharkey, J. 2008. Concise Book of Neuromuscular Therapy: a trigger point manual. Chichester, UK: Lotus Publishing. North Atlantic Books, California.
Sharkey, J. 2015. Letter to the Editor. Transmission of muscle force to fascia during exercise. Journal of Bodywork and Movement Therapies, 19(3) 391.
Sharkey, J. 2018. Biotensegrity-Anatomy for the 21st Century Informing Yoga and Physiotherapy Concerning New Findings in Fascia Research. Journal of Yoga and Physiotherapy. Volume 6 Issue 1. August. DOI: 10.19080/JYP2018.06.555680.
Sharkey, J 2019 a. Regarding: Update on fascial nomenclature-an additional proposal by John Sharkey MSc, Clinical Anatomist. Journal of Bodywork and Movement Therapies Volume 23, Issue 1, Pages 6–8
Sharkey, J. 2019 b. Biotensegrity focused Thiel Soft Fixed Dissection Course. Department of Anatomy and Human Identification, College of Life Sciences, University of Dundee, Scotland: https://www.ntc.ie/dissection-scotland/
Tomasek, J. J., Gabbiani, G., Hinz, B., Chaponnier, C., and Brown, R. A. (2002). Myofibroblasts and mechanoregulation of connective tissue remodelling. Nat. Rev. Mol. Cell Biol. 3, 349–363. doi: 10.1038/nrm809
Van der Wal, J., 2009. The architecture of the connective tissue in the musculoskeletal system- an often overlooked functional parameters as to proprioception in the locomotor apparatus. International Journal of Therapeutic Massage and Bodywork. 2(4), 9-23.
Category: Medical Massage
Tags: 2019 Issue #3