This clinical case was sent to the Journal of Massage Science by SOMI’s current student Brenda Howell, LMBT, MS. We think that this submission contains a lot of great information therapists can learn from.
However, three things caught our attention:
1. An extremely detailed patient’s examination Brenda conducted at the beginning, starting with visual evaluation. This is exactly what SOMI trains our students to do – always see the bigger picture and conduct soft tissue examination layer by layer.
2. A deep understanding of mechanisms behind the pathological changes Brenda registered. It is not enough to detect abnormalities in the soft tissues or body arrangement and try to fix them. Clear understanding of mechanisms behind their formation is the cornerstone of future clinical success. It gives the therapist the golden opportunity to constantly adjust treatment strategy.
3. Brenda very carefully and thoughtfully designed her treatment strategy for a very complex case with a variety of original and later developed clinical symptoms. It allowed her to correctly prioritize necessary therapies and slowly and carefully peeled off layers of somatic abnormalities one by one.
It is obvious that even at this point in her training Brenda exhibits full theoretical and clinical readiness to successfully practice Medical Massage therapy and help patients in the most desperate situation.
Dr. Ross Turchaninov, Editor in Chief
MEDICAL MASSAGE vs BODY TRAUMA
By Brenda Howell, LMBT, MS
North Carolina
Patient History
Accident at work occurred on July 12, 2011. While working, the patient reports that she was trying to push open a heavy steel door while at the same time (unknown to her) another person was pulling the door open. The second person was surprised to see her and let go of the door. The force of the door swung back towards the patient and hit left side of her body. The force of impact was so powerful that it knocked her across the room and into the opposite wall about 10-12 feet away. The patient was in excruciating pain. She underwent SAD with distal clavicle excision early 2012 and left ulnar nerve transposition in 2013. Since then the patient has had multiple rounds of PT that are both land and aquatic based.
Current Complaints
Patient experiences constant pain throughout her body that averages on the pain scale 8-9. She had so many areas of complaints that we decided to concentrate on her most pressing pain areas. During the Initial evaluation we focused on the pain and numbness that radiates from her cervical spine to the shoulders and mid back. We also focused on her severe headaches and blurred vision.
The patient describes the pain in the neck and middle back as fluctuating between sharp, aching, burning and pulsating. She specifically pointed to the following areas: between the C2 and C7 vertebrae, top of her head and supraclavicular fossae bilaterally. The patient also pointed to the pattern of pain radiation which refers from the area of C7 up her neck, over the top of the head and behind her eyes, forming a bilateral Cluster Headache. The pain is often accompanied by nausea and the sensation of heat which wrapped around the head and face. These sensations become very prominent when the headaches flare up.
She feels the sensation of constant pull in the front left of her chest when she even slightly turns her head or when she lifted her arms. She feels that her chest squeezed which affects her normal breathing.
The patient reported that her sleep pattern is deeply affected. She has difficulties falling asleep and she is unable to sleep through the night and as a result, she does not feel rested when waking in the morning and that is another contributing factor to the intensity of her symptoms. Even mild physical activities significantly increase pain intensity.
The patient also reported numbness and tingling sensations paravertebrally between C2 and C7. Numbness has spread bilaterally to her shoulders, and all way down to her wrists and hands. She also mentioned tingling sensations along her rib cage under her breasts and down both legs and to her feet.
Assessment
Visual Evaluation
The patient walked in heavily relying on her cane for support. She had difficulty sitting and standing and she held herself in a very guarded manner.
Both shoulders are rotated anteriorly and elevated. Her head was constantly held slightly to the right and a kyphotic curve in the upper thoracic is very prominent. The range of motion in her cervical spine was extremely limited. She could only move her head to the left and right a few degrees without causing extreme pain. Fig. 1 illustrates our patient’s initial cervical ROM.

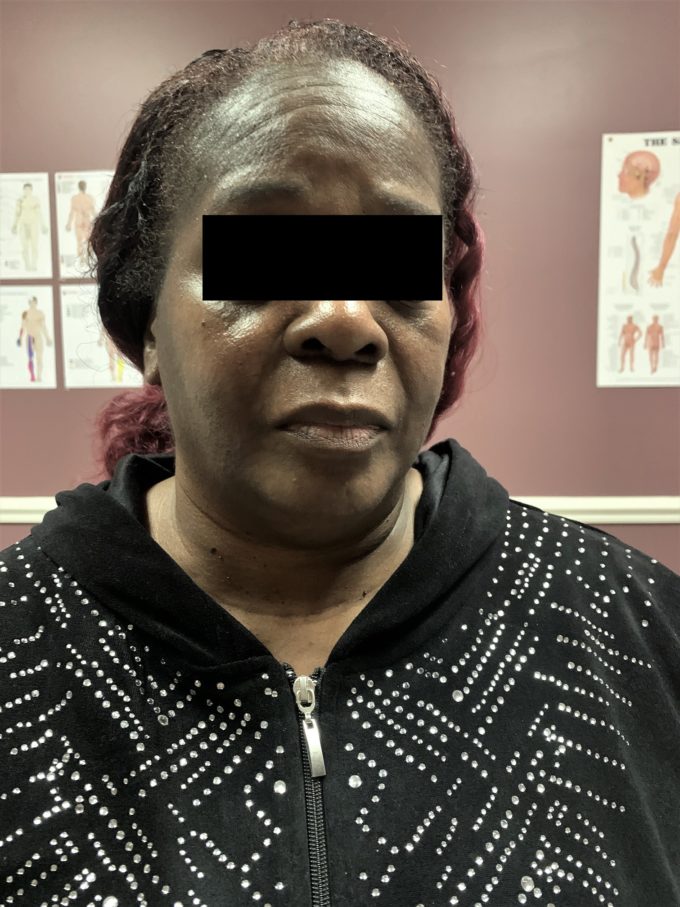
Fig. 1. Patient’s initial cervical ROM
The intensity of pain (patient pointed to the both supraclavicular fossae) increased dramatically with even slight movement of the head in flexion/extension. Technically, she can’t look both up and down. Visual signs of peripheral edema were present in the patient’s arms, hands (especially on the left side) and legs.
Interpretation of obtained data: As a reaction to the pain she suffered for so long her brain developed a very complex system of compensatory reactions in the form of dramatic postural changes and restriction in the ROM. The presence of the peripheral edema she didn’t have before indicates significant delay in the venous and lymph return, which is due to inactivity and in case of upper extremities due to the pressure on the subclavian veins in supraclavicular fossae
Sensory Test: During the application of the Sensory Test along the paravertebral lines the patient reported much more sensation on the right side compared to the left.
Interpretation of obtained data: Sensory Test conducted paravertebrally indicated the presence of cutaneous reflex zones on the left since the patient reported many more sensations on the right side with simultaneous stimulation of the skin across cervical and upper thoracic dermatomes. This reading may point to the irritation of the spinal nerves which innervated affected dermatomes on the left or compression of their terminal cutaneous branches by fascia and paravertebral muscles.
Cervical Compression Test (CCT) was conducted to examine the degree of tension build up within cervical segments and its results read as follows:
1st position (the head is in flexion, the patient looks down while CCT was applied) – pain wrapped around her head,
2nd position (the head in the neutral position, the patient looked straight forward while CCT was applied) – bi-lateral pain was reported on the lateral neck.
3rd position (the head is in extension, the patient looks up while CCT was applied) – the patient got an instant headache.
Interpretation of obtained data: The positive CCT in all three positions means that with time the patient developed significant pressure within cervical vertebral segments with intervertebral disks now contributing to the intensity of the symptoms. Positive CCT means that clinical response must be built carefully and gradually.
Wartenberg’s Test: Positive bilaterally, but on the left side the patient showed a greater amount of pain with just a very light touch.
Interpretation of obtained data: Even during clinical interview the patient pointed to the pain in both supraclavicular fossae. So, I fully expected a positive Wartenberg’s Test which indicates severe compression of the brachial plexus between anterior and middle scalene muscles. This tension is the obvious reason for peripheral edema present in both upper extremities due to compression of the subclavian veins by the anterior scalene muscle.
Examination of the Greater and Minor Occipital Nerves: Presence of severe Chronic Headache especially bi-lateral Cluster Headaches required detailed examination of the greater and minor occipital nerves. Compression Tests applied subsequently in the areas of possible entrapments of the greater occipital nerve by the Upper Trapezius, Semispinalis Capitis, Oblique Capitis Superior and the Oblique Capitis Inferior muscles indicated that all these areas were positive on the left side. On the right side the reading was much less intense.
Compression Test for the Minor Occipital Nerve behind the mastoid process was positive bilaterally.
Gernstein’s points were positive on both sides.
Eyeball Palpation Test was also bi-laterally positive.
Interpretation of obtained data: Testing indicated that the left greater occipital nerve was severely entrapped by all muscle layers it penetrated before reaching the scalp. There is also lesser degree irritation of the right greater occipital nerve.
Positive Compression Test for the minor occipital nerve explained tension build up in the temporal fossa on both sides.
Presence of the active Gernstein’s Points indicates significant tightening of the cranial aponeurosis which is an additional contributing factor to the Headache’s intensity and sensation of head squeeze our patient reported.
Eyeball Palpation Test indicated the presence of the Occipital-Trigeminal Convergence. In such case chronic irritation of the occipital nerves trigger the reflex irritation of the trigeminal nerve which in turn affects innervation of the soft tissues in the orbit. As a result, soft tissues which support the eyeball in suspended position tighten up and slightly push eyeball forward stretching the optic nerve and triggering Cluster Headache behind the eyes.
Chest Examination: Presence of the tingling sensation on the anterior aspect of her chest as well sensation of the pull in her chest when she moves her neck and arms guided me to the examination of her ribs and intercostal spaces.
I found that the patient was extremely sensitive when even mild pressure is applied along 1-6 intercoastal spaces, especially on the anterior surface of the chest.
Interpretation of obtained data: Chest pain is a result of patient chest impact and deformation occurred during the accident.
Treatment
Session outline: We have had a total of 11 sessions to date. Sessions are every Monday, Wednesday and Friday morning averaging 45 minutes a session.
The first 2 sessions focused on decompression of the soft tissues along posterior cervical spine by using a combination of effleurage, kneading, friction, stretching concentrating, techniques of relaxation of the paravertebral muscles and work on spinous processes of C3-C7 vertebrae. I also started to work carefully in suboccipital spaces on both sides trying to decompress greater and minor occipital nerves which were entrapped there.
On session 3 and 4, I included the Medical Massage Protocol for the left anterior scalene muscle along with the posterior cervical soft tissues’ decompression. Also introduced intercostal work on the anterior chest using Medical Massage Protocol for the Intercostal Nerve Neuralgia. Gave more attention to the suboccipital areas using Medical Massage Protocol for the Chronic Headache.
Session 7 I added Trigger Point Therapy in inhibitory regime enforced by electric vibration to the active trigger points in the trapezius and semispinalis capitis muscles.
Session 8 we were able to get her into a side lying position and work along the affected intercostal spaces with more precision, focusing on effleurage and friction on intercostal muscles and at their insertions into the two neighboring ribs, stretching of the intercostal muscles.
Session 9 I continued working on anterior scalene muscle while focused on the anterior aspects of the rib cage and suboccipital area, her scalp and area of her orbit.
By session 11 the intensity of original Wartenburg’s Test significantly diminished which indicated decrease of brachial plexus irritation.
Results
There is great pain reduction on the anterior and posterior neck and significant increase in the Cervical ROM. Wartenburg’s Test is mildly positive. Fig. 2 illustrates current Cervical ROM


Fig. 2. Current Cervical ROM in our patient
Also, we achieved significant control of her Headache and blurred vision she originally had almost gone.
As I mentioned above at sessions 5 and 6 I started the MMP for Intercostal Nerve Neuralgia and after the 9th session the patient (even though tender from the rib work) reported greater ease of breathing. There is significant decrease of peripheral edema on the left upper extremity.
She now stands straighter and her gait has become more fluid with less cane support. While the patient still has lots of work to do, each session is bringing her great improvements and more hope while continually increasing her quality of life. The patient’s entire life attitude changed, (she smiles a lot, she got new haircut etc.) and she is now more engaged and happily reports further improvements.

Brenda Howell began pursuing massage therapy to help her husband, a soldier who sustained injuries during his military service. She has personally experienced the frustration of going to doctor after doctor just to be told: “take these muscle relaxers and move on”.
Through her search for answers, Brenda began studying medical massage through the Science of Massage Institute in 2018 and is slowly learning the answers needed to help her clients and patients. She owns a multi-therapist practice in Fayetteville, NC and loves to learn new things as well as hike the wilderness in her spare time.
Category: Case Studies
Tags: 2020 Issue #1
