This post is intended for therapists who practice the clinical aspects of Massage Therapy.
Original Question:
Patient #1
Patient A experienced burning pain throughout the day and night in the right middle back for four months. The patient was unsuccessfully treated by DC, PT, and a massage therapist who practiced clinical massage.
Patient #2
Patient B suffered burning pain along their left upper extremity, especially along the dorsal surface of the first and second fingers, and moderate peripheral edema throughout their left upper extremity.
After examining both pictures, what can be deduced about both patients? What clinically unites both patients and what is the most likely cause of their symptoms?
The therapist practicing massage therapy’s clinical aspects must read the patient’s body like an open book. The body constantly feeds therapists with priceless clinical data which must be read and interpreted correctly—a true foundation for responsible Medical Massage Practice. That is why SOMI’s Medical Massage training program dedicates so much time to teaching therapists these critical clinical skills.
Thank you for all your responses. Readers offered various solutions to the posted questions:
1. Different Trigger Points indicated
In most cases, if there is no previous trauma, active TPs are not the cause but rather the consequence. The active TP in skeletal muscles will never give patient skin Burning Sensations and hair loss. The active TPs in skeletal muscles were present in these patients, but they have no connection to visual changes in the pictures.
2. Tension in rotator cuff muscles as well as Frozen Shoulder
There are no anatomical or pathophysiological indicators either patient suffered from Frozen Shoulder. This is a completely unrelated pathology.
3. Thoracic disk degeneration following spinal nerve compression. Osteophyte (a.k.a. on thoracic vertebra)
Yes, there is a chance of that happening. However, in contrast with cervical and lumbar disks, thoracic disks have a much lesser chance of degeneration and compression of the thoracic spinal nerves. The ribs always unload vertical compression forces within thoracic segments, especially if the patient is relatively young. Finally, if the thoracic disk compresses the spinal nerve, the pain should radiate along the affected dermatome to the patient’s lateral and anterior body. We didn’t mention that.
4. Gallbladder disfunction
Yes, there is the possibility of similar changes in the middle back in cases of gallbladder dysfunction formed secondarily. However, gallbladder dysfunction must be diagnosed by an internist or gastroenterologist first, not vice versa. In medical practice, diagnosis of any visceral abnormality is not established based on soft tissue dysfunction or on reflex zone presence. The therapist should consider these visual changes as signs of reflex zone formation after the internist or gastroenterologist diagnoses gallbladder dysfunction.
5. Tinea corporis
Tinea corporis is a ringworm fungal infection. The patient will show skin lesions in the form of a red circle with a red raised border and normal skin color and structure inside the ring. There are no signs of that in both pictures.
6. Herpes infection
Herpetic infection indeed will trigger burning pain. However, acute herpetic infection supposes to have skin lesions, or they should appear around two weeks after the onset of the pain. If that was the case, we mentioned that in the question. Also, in acute shingles, there is no local hair loss. In chronic herpetic infections, local hair loss is possible but very rare, and it MUST be accompanied by skin pigmentation at the places when lesions chronically reappear.
ANSWER:
The formation of Cutaneous Reflex Zones with burning pain and local hair loss unites both patients. In both patients, Cutaneous Reflex Zones formed due to chronic irritation of cutaneous nerves, which support the innervation of the skin in the affected areas.
Patient #1.
Patient #1 complained about a chronic burning sensation in the middle back, which he feels throughout the day and night. This clinical sign is explicitly attributed to cutaneous trigger points. However, this patient’s most striking indicator of cutaneous reflex zones is local hair loss along the T8-T9 dermatomes, supported by compressed cutaneous nerves. Cutaneous branches of the thoracic spinal nerve are compressed between the soft tissues of the spinal grove. Fig. 1 illustrates the dermatomal map and corresponding cutaneous branches supporting each middle back dermatome.
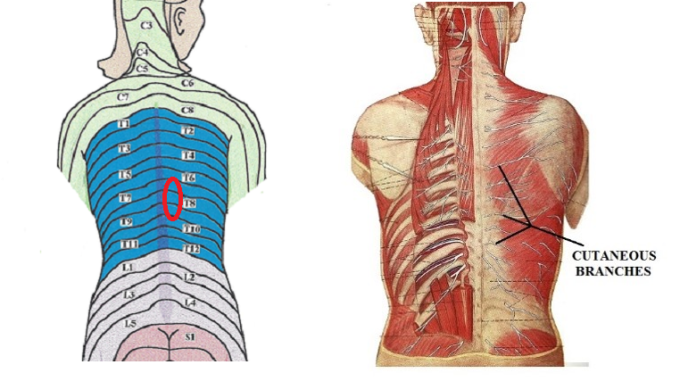
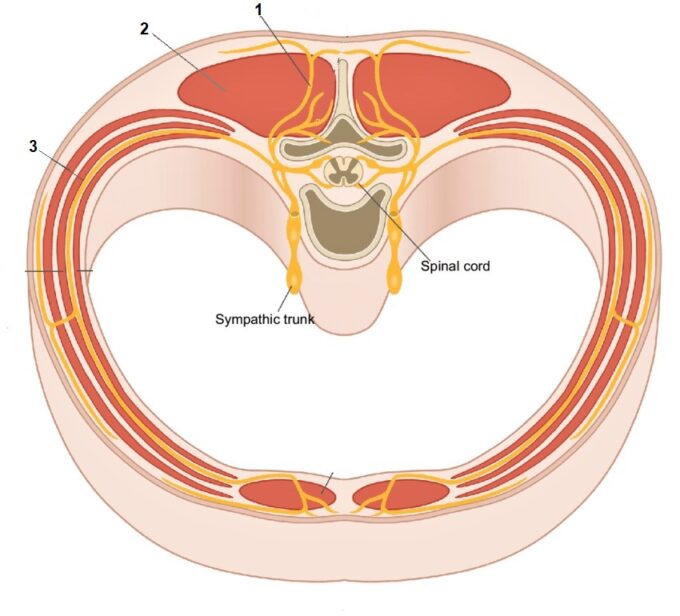
The cutaneous branches of the thoracic spinal nerves need to pierce the soft tissues of the middle back to get under the skin to innervate corresponding dermatomes. Fig. 2 illustrates the anatomical pathway of compressed cutaneous nerves.
Why did the patient experience hair loss? When cutaneous nerves are irritated and compressed, the normal support of the skin and superficial fascia is severely compromised, and it weakens hair follicles which fall out first.
From the treatment perspective, this patient was treated with decompression of superficial fascia covering the lower portion of the trapezius muscle, especially in the spinal groove where cutaneous branches emerge under the skin to provide its innervation. The next step was decompressing the middle fascia, which separates the trapezius muscle from the spinalis dorsi and longissimus dorsi muscles using Trigger Point Therapy and Muscle Energy Techniques. Each session was finished with skin kneading and superficial friction in the affected parts of the skin to address cutaneous reflex zones.
Patient #2
This patient exhibited hair loss along the radial forearm and thumb (compare both sides). This hair loss happened due to a combination of two factors: irritation of the radial nerve (radial nerve neuralgia) and peripheral edema formed on the forearm and hand due to insufficient venous drainage from the left upper extremity. The left wrist and hand are visibly swollen compared to the right side, and the skin has a brownish color.
These two factors are not separate events but result from the same initial trigger – tension in the anterior scalene muscle, which has irritated the radial nerve and simultaneously compressed the subclavian vein, delaying venous drainage from the entire left upper extremity. Thus, the patient exhibited a blooming picture of Thoracic Outlet Syndrome, a combination of neurological and circulatory abnormalities.
From the treatment perspective, the only solution for this patient was an application of the Anterior Scalene Muscle Medical Massage protocol to free the radial nerve from irritation and eliminate pressure on the subclavian vein to restore proper drainage from the upper extremity.
Please join SOMI in two upcoming Medical Massage Seminars and Webinars in 2023: Medical Massage Courses & Certification | Science of Massage Institute » Medical Massage Continuing Education
Category: Blog

