by Ross Turchaninov, MD
In the previous JMS issues, we explored the anatomy and physiology of the periosteum and the mechanisms behind the formation of periosteal dysfunctions.
The following article continues the conversation touching on types of periosteal dysfunctions therapists may encounter daily.
Trauma, overuse, or reflex zone formation will show up as structural changes in the periosteum at specific locations along the bone. Periosteal dysfunctions will never appear in the parts of the bone covered by layers of soft tissue and will instead form only in the areas where the bone is covered just by the skin. For example, there are no periosteal dysfunctions in the femoral shaft, but they will form in the parts of the femur covered just by skin such as the greater trochanter, around the knee joint (lateral and medial condyles of the femur). Other possible locations of periosteal dysfunctions include the entire ulna or anterior tibia, the medial edge of the scapula, and the spinous processes of the vertebrae, among others.
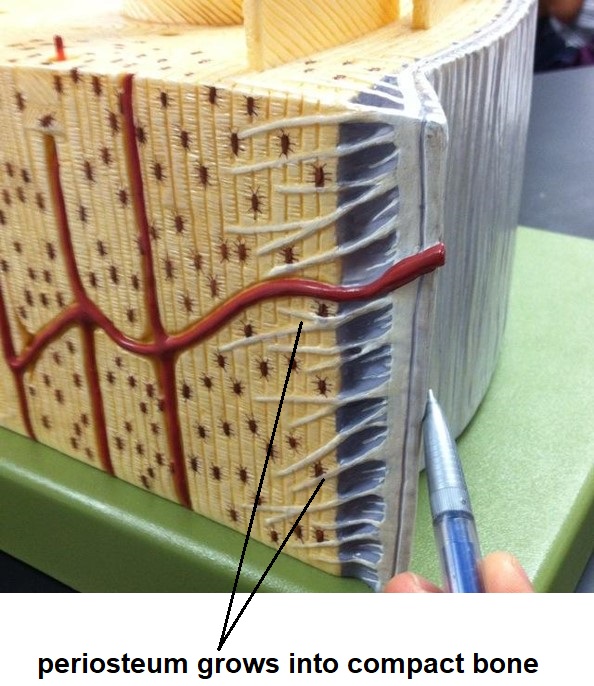
From an anatomical perspective, skin-only covered areas of bone are points of stability for soft tissue insertion such as tendons, ligaments, and joint capsules. As discussed in the first part of this article in the previous issues of JMS, soft tissues insert into the periosteum and the periosteum grows inside of the bones using Sharpey’s Fibers to stabilize itself. In soft tissue insertion areas, the periosteum is at an anatomical and physiological disadvantage even during normal functioning. The following additional disadvantages create a perfect storm for periosteal dysfunctions:
- Significant risk of direct trauma to the periosteum in areas not covered by layers of soft tissues.
- Lower oxygenation of the periosteum in these areas since circulation is limited only to the skin. For example, in the femur shaft, oxygenation of the periosteum’s outer layer is supported by powerful muscles which have abundant local circulation. However, around both condyles that form the knee joints, soft tissue layers are thinner and they don’t deliver less oxygen needed for the diffusion process. This process of diffusion is one of the main sources of the periosteum’s oxygenation.
- In these areas, the robust soft tissues that support locomotion elicit significant contractile and stabilizing forces, stressing the periosteum.
Periosteal dysfunction can be separated into three categories:
- Periosteal inflammation with periosteal trigger point formation
- Partial periosteal detachment
- Periosteal irregularities and bone spur formation
PERIOSTEAL TRIGGER POINTS (PTP)
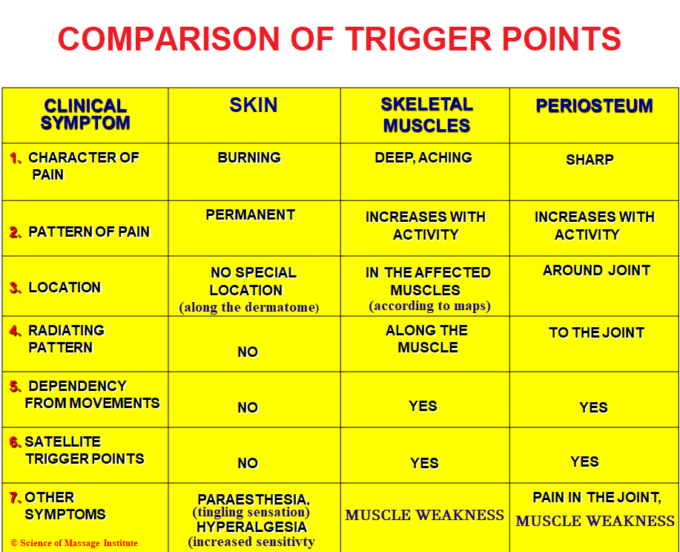
Three types of Trigger Points (TPs) can form in the human body: cutaneous TPs in the skin, TPs in skeletal muscles, and periosteal trigger points (PTPs). Each TP type has a unique clinical picture and requires individualized treatment. Fig. 1 below summarizes the clinical symptoms associated with each type of TP.
PTPs are the epicenters of periosteal inflammation and are more painful than TPs in the skin and skeletal muscles. Since they are located mainly around major joints, the pain they trigger tends to radiate throughout the joint, mimicking the clinical picture of Osteoarthritis (OA). In such cases, patients present symptoms undistinguishable from real OA. Only a detailed palpatory evaluation will clarify active PTPs as the real cause of the patient’s joint pain. Thus, some patients mistakenly diagnosed with Osteoarthritis will completely recover from joint dysfunction after Medical Massage eliminates periosteal inflammation.
Active PTPs also cause significant muscle weakness because each muscle contraction stresses already inflamed periosteum causing acute pain. Therefore, muscle weakness results from patients trying to reduce or avoid movements that may trigger pain and discomfort.
Periosteal TPs can be further categorized according to the intensity of pain and dysfunction:
- A Leading PTP is an area of the periosteum with the highest pain intensity and dysfunction. Usually, the patient will pinpoint this area. Applying mild pressure to the Leading PTP will trigger acute pain, and the patient will quickly withdraw that body part.
- Supporting PTPs of the First Type are less painful during a palpatory evaluation and are located around the Leading PTP. They usually form later as a local periosteal reaction to chronic inflammation.
- Supporting PTPs of the Second Type are located on the opposite, unaffected side but in the exact location of the Leading PTP on the affected side. This PTP is less sensitive than the previously described PTPs and is often identified during a palpatory evaluation rather than a patient’s complaints. Supporting PTPs of the Second Type are present ONLY in cases of chronic periosteal inflammation and the long-lasting presence of active PTPs. The formation of periosteal inflammation on the unaffected side is a classic example of reflex zone formation.
PARTIAL PERIOSTEAL DETACHMENT
The presence of chronic inflammation in the periosteum weakens its attachments to the underlying bone. Powerful muscle contraction may damage Sharpey’s Fibers, and it causes partial detachment of the periosteum in the place of muscle insertion. Such partial detachment causes acute pain even during mild muscle contractions. Fig. 2 illustrates periosteal detachment and strain of Sharpey’s Fibers.
Clinically, it can be so intense that a patient with Tennis Elbow–a classic example of periosteal dysfunction–cannot even hold a cup of coffee. At some point, periosteal detachment can be so advanced that it is impossible to make clinical improvements with Medical Massage. Only surgical re-attachment of the soft tissues and periosteum to the bone can be a viable solution. That is why therapists must familiarize themselves with the correct treatment strategies to prevent irreversible damage.
BONE SPURS
Bone spurs are the final and irreversible step in periosteal dysfunction. The first part of this article, shared in the previous issue of JMS explained that the periosteum is made up of two layers–an outer connective tissue membrane and an inner layer of cells called osteoblasts. These cells are responsible for healing fractures and forming new bone. Unfortunately, this same healing mechanism is also responsible for painful bone spurs.
A bone spur, or osteophyte, is an outgrowth from the bone. Spurs accompany advanced OA stages or can result from direct periosteal trauma. Aside from the loss of cartilage triggered by OA, bone spurs are another contributing factor to acute pain accompanying joint degeneration. When spurs form, soft tissues start to rub against the sharp tips of the spurs, triggering additional pain with each movement, soft tissue inflammation, and, as a result, extra protective muscle tension.
Let’s dive into the formation of bone spurs using knee joints as an example. A patient suffers from mild pain on the medial aspect of the knee joint due to the tension developed in soft tissues (muscles, tendons, fascia, etc.). This newly developed soft-tissue tension elicits extra pressure at the insertions into the periosteum, causing its mild irritation. This chronic soft tissue tension activates some osteoblasts, and periosteal inflammation forms there. When osteoblasts became active, they immediately went to work, confusing chronic inflammation with a bone fracture. These activated osteoblasts start to produce and deposit collagen, which then mineralizes and becomes new bone forming the bone spur. The only difference is that the inflammation resulting from chronic tension in the soft tissues is way smaller than trauma during the bone fracture. Thus, a smaller number of osteoblasts become active, slowly contributing to new bone deposits along the force applied to the periosteum by tensed soft tissues. That is why spurs have very sharp tips that follow the direction of pressure applied to the periosteum by tensed soft tissues. Fig. 3 illustrates the different locations of bone spurs. Notice that osteophytes formed in the direction of soft tissues insertions to the periosteum.

a – bone spurs formed along the edge of the tibia (X-Ray picture)
b – Heel spur on the bottom of the calcaneus (X-ray picture) c – bone spurs on the anterior surface of the lumbar vertebrae (3-D MRI image)
In the early stages of periosteal dysfunction, Medical Massage can eliminate PTPs, avoid the formation of bone spurs later in the patient’s life and prevent or slow down OA development. In the following article, we will discuss the palpatory evaluation of Periosteal Dysfunctions.
Join SOMI’s Webinar: Medical Massage Concept: From Theory to Clinical Application, on April 1-2. You will get absolutely fascinating professional knowledge and evaluation skills while getting 8CEUs! Here is the link to SOMI’s LIVE Webinar: Medical Massage Courses & Certification | Science of Massage Institute » SOMI’s Webinar April 1-2, 2023
About the Author
To read Dr. Ross Turchaninov’s Bio please click here: Medical Massage Courses & Certification | Science of Massage Institute » Editorial Board
Category: Medical Massage
Tags: 2022 Issue #3