A very frequent complication of surgery is direct trauma of the cutaneous nerves or their compression from resulting scar tissue. Both unfortunate scenarios may trigger a condition called hyperesthesia. Hyperesthesia is associated with an abnormal increase in sensitivity to touch and pressure. Such stimuli will trigger electric shock type of sensations in the affected areas. Some patients may also complain about numbness, tingling, and burning sensations. These extremely uncomfortable symptoms may last for months, years, and sometimes for the rest of a patient’s life.
Tianna Beebe, LMT from Appleton, Wisconsin, and a current student of SOMI encountered this complicated pathological situation at the beginning of 2023. The patient had suffered from postsurgical nerve trauma for months before Tianna brought her to almost complete recovery, using a combination of Medical Massage and the application of Essential Oils.
Notice how masterfully she developed and managed a treatment plan, from lymphatic drainage and scar tissue stretching to slowly desensitizing the affected nerves and resetting the patient’s sensory cortex. Also, please pay attention to how meticulously she recorded her patient progress. This case is an excellent illustration of an important fundamental concept of Medical Massage: building clinical response.
Dr. Ross Turchaninov, Editor in Chief
MEDICAL MASSAGE WITH AROMATHERAPY vs POSTSURGICAL NERVE TRAUMA
By Tianna Beebe, LMT
Appleton, Wisconsin
A 64-year-old woman presented with significant numbness and pain in her right thigh and right lower abdominal quadrant following complex surgery performed in June 2022. Very frequently throughout the day, she experienced electric shock-type pain in the areas of both incisions. Here is a list of her surgical procedures:
- Right retroperitoneal dissection
- Right common and external iliac artery endarterectomy with the removal of foreign body (stent)
- Percutaneous cannulation of the right common femoral artery
- Right external iliac artery bovine pericardial patch angioplasty
- Right common femoral and superficial femoral endarterectomy
- Right superficial femoral artery bovine pericardial angioplasty
Surgeries were performed with two incisions; one in the lower right quadrant of her abdomen and another in the right upper anterior thigh.
Beginning ten days after surgery, she had weekly 90-minute massage sessions for three weeks, then every two weeks for the next five months, to address tension and stress, with no intentional focus on the loss of sensation in her legs and abdomen. No significant clinical progress was made in the affected areas.
In January 2023, we began targeted treatment to address her symptoms with a combination of Medical Massage and Aromatherapy using Peppermint essential oil (EO) three times per week with 30-minute sessions.
1st Session:
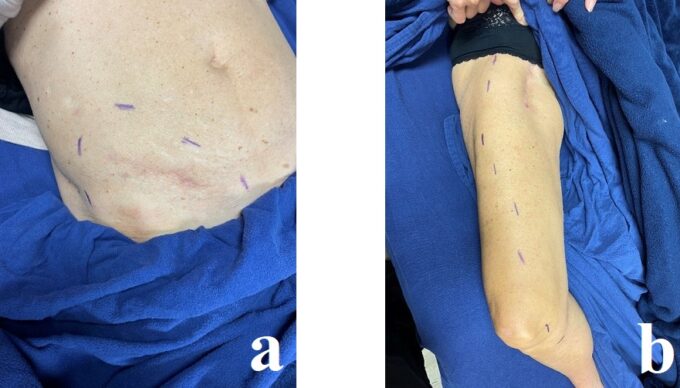
I started the session by marking the borders of the affected areas, using a Sensory Test (gentle scratch with my fingernail) to determine the distribution of numbness or sensory deficit that she felt along the affected dermatomes. Results are presented in Fig. 1.
Fig. 1. Borders of areas with sensory deficit
a – Borders of numbness in the lower abdomen
b – Borders of numbness in the thigh. In this picture, my patient’s index finger points to the upper point of the sensory deficit on the upper thigh
I started lymphatic drainage from the foot up to the knee for two minutes, then from the knee to the top of the thigh for two minutes, avoiding direct contact with compromised areas. Before working directly on the affected regions, I mixed three drops of Peppermint EO with a small amount (dime size) of lotion. I started to use draining effleurage strokes with light pressure along the affected areas and correlated the speed and intensity of my strokes with the patient’s sensations.
I added light cross-fiber friction along the adductors for six minutes, moving from the medial to lateral aspects of the thigh, followed by effleurage. The patient reported a warm sensation from the Peppermint application.
I shifted my attention to the scar on her upper thigh, applying cross-fiber friction for four minutes. She immediately reported the electric shock-type of pain when even mild pressure was applied directly to the medial side of the scar. She also reported a sensation of tingling down to her toes. The pain stopped as soon as I eased the pressure of my touch.
I started to work in the lower right quadrant of her abdomen, applying the same mixture of lotion and EO in a clockwise direction for one minute. I also used draining effleurage from the median line of the abdomen to the anterior superior iliac spine (ASIS) across the affected area for seven minutes.
Finally, I concluded the session with cross-fiber friction to the scar in the lower abdomen for two minutes. The patient again reported electric shock sensations that wrapped around her waist.
2nd Session:
There were no changes in the Sensory Test results compared to the previous session. However, the patient reported that her right leg and abdomen had felt different since the last session, specifically less intense electric pain in her right leg. I followed the same treatment protocol.
3rd Session:
The patient reported a flare-up the previous night, experiencing several burning sensations and electrical shocks down her right leg to her big toe. I started with the same protocol. When I applied even mild pressure on the medial edge of her rectus femoris muscle (the spot indicated in Fig. 2), she felt intense, ‘exploding’ electric shock radiating pain down along the medial leg all along the way to her toes.
Fig. 2. Area in the rectus femoris muscle where mild pressure irritates branches of the femoral nerve
During this session, I added work in the patient’s lower back, using simultaneous counter-pressure with my left hand on the spinal erectors near L5 and the sacrum while my right-hand applied pressure around the ASIS. She reported fewer tingling sensations during the cross-fiber friction on the scar located on her thigh.
4th Session:
The patient reported that her right leg was feeling much better: overall, more sensation and less intense electric-type pains. She did notice a new discomfort in her right groin and sciatica-like pain down the back of her right leg; however, she was sleeping better and, for the first time, didn’t wake up in the middle of the night.
I started the session with a sensory test on the dermatomes of her abdomen and thigh, noting definite improvement in restoring normal sensation. I added Myofascial Release on the rectus femoris this time, followed by light repetitive kneading. She felt some electric sensation when I used cross-fiber friction on the thigh scar and reported tingling on her right side, including previously completely numb areas.
5th Session:
Again, the patient reported the flare-up during the night after the last session. Subsequent nights she slept well. Sciatic-like pain and a burning sensation in her lower abdomen were still there.
The following additions were made to the previous treatment protocol:
- Lymphatic drainage massage on foot to her knee. Three minutes later, the burning sensation on her foot had subsided.
- Two drops of Sandalwood EO and three drops of Copaiba EO, diluted in lotion.
- Scar mobilization techniques on the thigh, with which she immediately noticed fewer electric shocks.
6th Session:
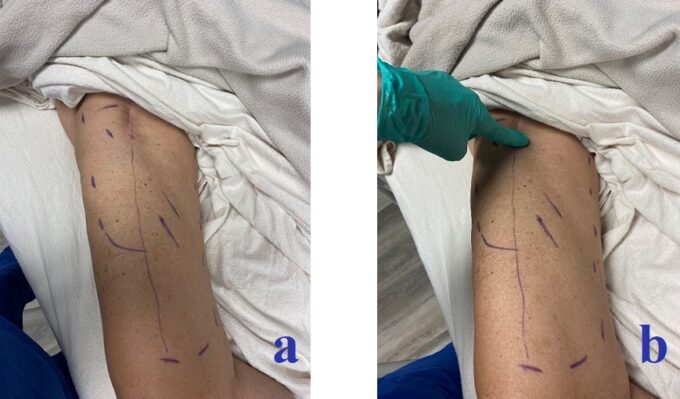
The patient said her leg felt 50% better and suffered no flare-ups after the previous session. While she had less pain overall, there was still some tingling and numbness; however, nowhere near the intensity as before, and her pain level did not distract her from everyday activities as it had. She noticed that sensations completely normalized around and immediately above her right knee. She’d slept well before coming in. Fig. 3 illustrates the patient’s progress.
Fig. 3. Patient’s progress:
a – Outer dotted line indicates where the patient felt almost full recovery of sensations; the vertical line on the anterior thigh indicates an area where the patient started to feel the return of some sensations; two diagonal lines on the medial thigh indicate an area where the patient was beginning to feel tingling instead of complete numbness.
b – My index finger indicates an entirely numb area at the lower portion of the scar.
c – Dotted line indicates a decrease in skin numbness (compared to Fig. 1) around the scar in the lower abdomen.
The skin over the anterior upper third of the thigh was hypersensitive and the gracilis muscle was very tender during palpation. Her pectineus muscle was tight as well, and palpitating it sent electric shock pain through her scar.
For this session, I started to increase the intensity of treatment, applying medium pressure to the lateral portion of her quadriceps, which didn’t trigger any nerve pain. However, she reported some small amplitudes of electric shocks down to her groin while I was using effleurage in the right lower quadrant of her abdomen.
I also used Neuromuscular Therapy techniques along the vastus lateralis and lateral portion of the rectus femoris to address the dent in her anterior thigh muscles that had formed after surgery. No electric shock pain was reported when cross-fiber friction was applied at the bottom of the thigh scar. Again, I added three drops of Copaiba EO and two drops of Sandalwood EO to the lotion when I worked on her right foot and lower leg.
7th Session:
The patient reported feeling much better after the 6th session, since she had only one incident of electric shock pain from the groin all way down to her great toe. She had done a lot of walking during the weekend.
There was full restoration of normal innervation of the skin in the lower right quadrant of her abdomen. She reported a significant increase in ability to feel, touch, and tolerate pressure on her thigh. The Sensory Test confirmed a significant reduction in the size of areas with sensory deficit. Also, she noticed increased muscle strength in the right leg and during the day she was able to take fewer rest breaks.
I continued to gradually increase pressure during various strokes. The anterior aspect of the thigh had almost completely restored normal innervation. The area over the pectineus muscle still triggered electric shocks but they were tolerable. When I started to work on the areas which were still numb, the patient didn’t report even mild electric shocks, nonetheless, I kept my pressure light in those areas. The upper part of the thigh scar was still very sensitive during scar mobilization strokes, triggering electric sensations but with lesser intensity. At the end of the session, I worked on her abdominal scar and its mobilization triggered pain referral to her external oblique and to the bottom of her right rib cage.
8th Session:
The patient reported tingling sensations from the upper thigh all way to the lower leg. I followed the same protocol as before with a gradual increase of pressure. Instead of the electric pain, she felt tingling sensations along the inferior aspect of the gracilis, inferior border of the pectineus, and around the inferior aspect of her scar. She reported having more sensitivity around the thigh scar. Fig. 4 illustrates the patient’s progress.
Fig. 4. Patient’s progress:
a – Decreased numbness on the anterior thigh (compare to Fig. 1).
b – Complete restoration of skin innervation in the lower abdomen.
9th Session:
Patient reported that she did not have any foot or leg pain since the last session. She did get a couple of mild shocks, but they only went to her knee. She could now feel the area above the scar in her entire groin area which was previously numb. Interestingly enough, I hadn’t even worked in her groin!
Sensations along the dermatomes in the lower quadrant of her abdomen, including the scar itself, were completely restored. Her ability to engage in daily activities had greatly improved and her lower extremity regained significant strength.
This time I used firm, medium pressure throughout much of the session and also gently increased pressure, even in the more sensitive area of the upper medial thigh. During the cross-fiber friction along the gracilis and pectineus, she had only mild local electricity without referral pain anywhere.
The only locally sensitive area remaining was on the inferior aspect of the scar. Originally the patient had a large seroma in this section of the scar after the surgery. I applied 1 drop of Sandalwood EO and 1 drop of Copaiba EO to the lower leg.
Conclusion:
The patient had experienced postsurgical trauma of the sensory and motor branches of femoral nerve with development of severe hyperesthesia and muscle weakness. Medical Massage in combination with Essential Oils decompressed scar tissue of the femoral nerve and allowed the sensory and motor branches to gradually restore normal functions.
The frequency of the Medical Massage sessions with special techniques of scar tissue decompression and the use of Peppermint EO gave us clear, beneficial clinical results. There is mounting evidence that Peppermint EO has neuroprotective effects. (https://www.sciencedirect.com/science/article/pii/S0753332222009489). My patient is extremely happy with the treatment outcome and her almost full recovery.
ABOUT THE AUTHOR
Tianna’s love of people, service, and helping others find solutions drove her to pursue her desire for learning and deepen her knowledge of the human body by receiving her Massage Therapist Technical Degree from the Fox Valley Technical School in December 2019.
Tianna then received her national board certification through the National Certification Board for Therapeutic Massage and Bodywork in January 2023. Before becoming a licensed massage therapist, she had seven years of running a small wellness business focused on essential oils.
Tianna is a student at Aromahead Institute and a Medical Massage student through The Science of Massage Institute. She hopes to complete her certifications in these two modalities by 2025, as they take considerable time to complete. She is skilled in Myofascial Release, Neuromuscular Therapy, Essential Oil massage, and customizing each session to the client’s needs. She is owner of Bridge Massage & Wellness Clinic in Appleton, Wisconsin and can be reached at (920)257-8391
Tianna loves being outside, active, burying her nose in a scientific book, being involved in the community and with her church, and being a wife and mother.
Category: Case Studies
Tags: 2023 Issue #1