By Dr. Ross Turchaninov,
Phoenix, AZ
Why should we dedicate a special article to the subject of Hyaluronic Acid (HA), which seems to be unrelated to massage therapy and manual medicine? We deem this topic important because scientific and clinical data from the last 10-15 years indicate that HA directly correlates with Myofascial Pain Syndrome and its role in Medical Massage therapy for delivering stable clinical outcomes. This article presents a review of the exceptional scientific publication entitled “Hyaluronan and the Fascial Frontier” by Rebecca L. Pratt in the International Journal of Molecular Sciences (2021).
WHAT IS HA AND WHY DO HUMAN BODIES REQUIRE IT?
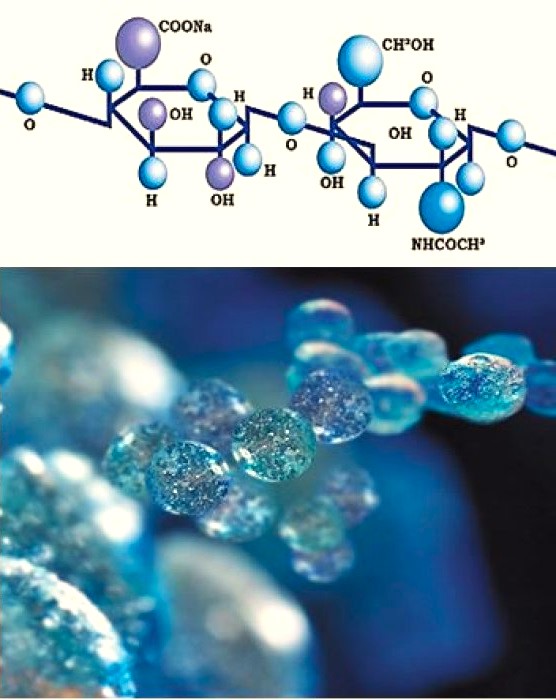
HA belongs to a family of special sugars distributed in all living tissues – glucosaminoglycans. As a negatively charged molecule, it has a particular affinity to water, and it is able to retain it in large quantities. This feature gives HA high viscosity. Even though our bodies contain only 15-16 grams of HA, it plays a vital role in healthy bodily functions and, therefore, our health. Fig. 1 illustrates the chemical formula of HA.
Although HA was discovered decades ago (Meyer and Palmer, 1934), it took medical science some time to fully understand its critical role. Only recently has scientific data directly linked HA to medical massage and manual therapy.
These are important body functions commonly associated with HA:
- Synovial fluid lubricates all joints and protects our hard-working cartilage. Due to water retention and high viscosity, HA decompresses cartilage, thereby working as an initial shock absorber. It also scavenges free radicals and various debris accumulated in joint cavities (Laurent, 1996),
- Supports extracellular matrix (i.e., spaces between individual cells)
- Wound healing
- Beauty Medicine to support skin turgor.
BREAKING NEWS FROM ITALY
In 2011 a group of Italian scientists led by Dr. Carla Stecco published a fascinating paper regarding HA. Generally speaking, medical science has studied the human body in great detail and is now investigating specific genes. Despite thinking that we knew almost everything about organs, tissues, and even individual cells, Dr. Stecco and her team proved us wrong because they discovered a completely unknown type of cell in the fascia. They called it – fasciocytes. These cells are closely related to the fibroblasts which produce collagen. However, fasciocytes look different and, what is more important, they are HA production stations.
Why is all of this so important to the therapists who work in somatic rehabilitation? It completely changes the dynamic of our treatment strategy. This discovery directly linked the origin of Myofascial Pain with insufficient HA production, loss of fluidity, insufficient fascia lubrication, and eventually fascia scarification. If the production of HA was affected and fluidity was to be lost, “the behavior of the entire deep fascia and the underlying muscle would be compromised” (Stecco, 2011).
It is important to note that each skeletal muscle is in a fascial envelope that covers all of its surfaces. This is why, without total decompression of the superficial and deep fascia, work on the skeletal muscles alone will NEVER deliver stable clinical results. If the envelope remains too short, hypertonic muscle abnormalities (hypertonus, trigger point) will always return. Thus, fascial tension is essential and frequently overlooked with the local mechanism of Myofascial Pain Syndrome.
Another study by Fede et al. (2021) demonstrated how important HA is for the normal function of the fascia and illustrated the unequal distribution of HA among different fascial planes in the human body. More HA is registered in the fascia which covers powerful muscles with a large range of contraction, and less HA is registered in muscles with lesser contractile ability. For example, healthy fascia, which covers muscles on the anterior thigh contains up to 35 mg/g of HA, while fascia, which covers the trapezius muscle contains only 6 mg/g of HA. Quadriceps engaged in extensive isotonic contractions need more HA for lubrication of their fascia than the fascia that covers the trapezius muscle, which mostly works in the isometric regime.
Another essential aspect of HA is its inner structure. HA molecules exist in two forms: long- and short-chained. Long-chained HA molecules lubricate healthy fascia, while tense fascia, which loses its elasticity and eventually forms adhesions, is lubricated by short-chained HA. Their self-sticking nature is responsible for the decreased mobility of fascial fibers and, eventually, underlying myofibrils (Matteini et al., 2009).
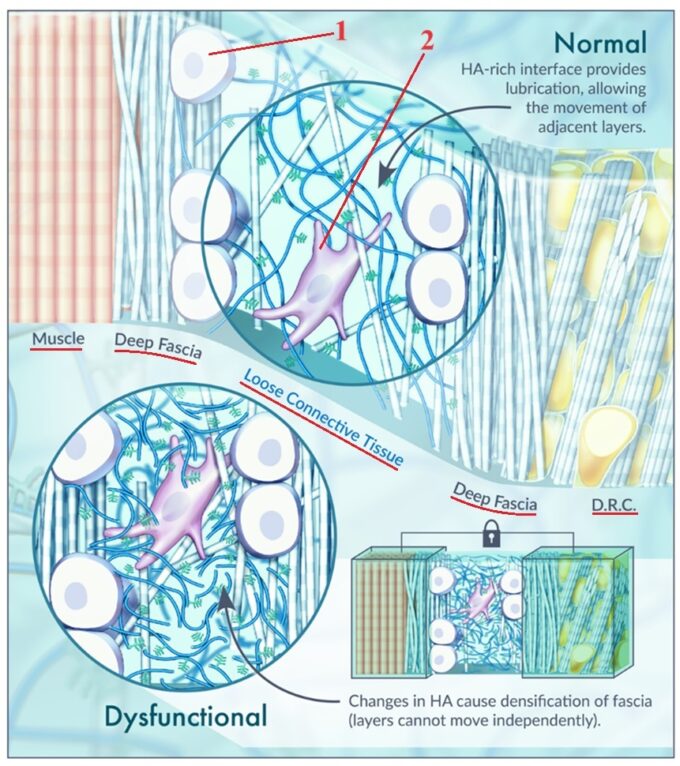
Let’s look at a fascinating diagram (Fig. 2) of the structure of healthy and damaged fascia from the article we are reviewing here (Pratt, 2021).
In the upper part of this diagram, you see the structure of healthy deep fascia arranged in layers. On the upper left, you see deep skeletal muscle covered by an inner layer of deep fascia. This inner layer contains large round-celled fasciocytes (#1 in Fig. 2) that produce HA. The next layer of the deep fascia is loose connective tissue containing large cells called fibroblasts (#2 in Fig. 2) responsible for fascia repair. The long blue lines around the fibroblast are long-chained, healthy HA molecules that provide normal fascia lubrication. Then we have the outer layer of the deep fascia, and it again contains fasciocytes that produce HA. D.R.C. stands for deep retinaculus cutis, which are fibrous bands running from the skin dermis to the underlying fascia. They give soft tissue its stability.
In the lower part of the diagram, you see the early stages of unhealthy deep fascia. The only difference at this point is the replacement of long-chained HA molecules with short-chained HA molecules (short blue lines). As discussed above, short-chained HA molecules are observed in tense fascia BEFORE fascial adhesions and scarification forms.
Replacement of the normal long-chained HA by short-chained HA triggers fascial tension, adhesions, and fascial scarification. These pathological changes dramatically affect the health and performance of underlying skeletal muscles. Figures 3 and 4 illustrate endoscopic pictures taken during surgery of healthy and damaged fascia.
Fig. 3. Endoscopic picture of healthy fascia (Carro et al, 2016)
Fig. 3 presents a live endoscopic picture of the healthy deep fascia, which covers vastus lateralis part of the quadriceps muscle (‘b’ indication in the picture) at its origin at the periosteum of the upper femur. The powerful, thick tendon (‘a’ indication in the picture) seen at the bottom of the picture is the tendinous part of the gluteus maximus muscle at its insertion into the periosteum of the femur. Notice the smooth, pearl-colored appearance of the healthy, deep fascia and many droplets of HA-based lubrication.
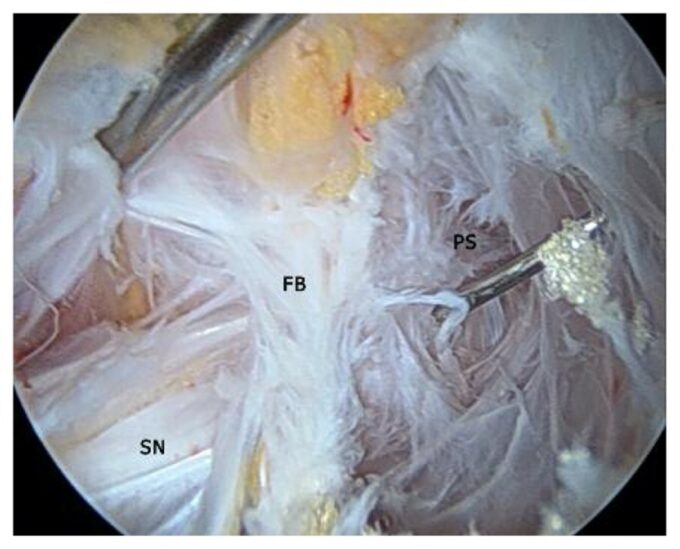
Fig. 4. Endoscopic picture of the damaged and scarificated fascia (Carro et al, 2016)
Fig. 4 presents a live endoscopic picture of the damaged and scarificated deep fascia, that covers piriformis muscle (PS indication in the picture). The scarification of the fascia was so advanced that it formed a fibrotic bridge (FB indication in the photo), which entrapped the sciatic nerve (SN indication in the picture). The fascia over piriformis muscle completely lost the smoothness and regularity of the healthy fascial fibers, and instead, it became an irregular network of scar tissue. Another critical aspect is the complete absence of the fascia lubrication.
Such intense damage to the fascia frequently results from deep tissue pressure during various types of bodywork. In these cases, the misinformed therapist with all good intentions uses excessive pressure during the therapy, triggering fascial de-lubrication with the following adhesions and fascia scarification.
In Part II of this article, we will discuss the impact that this vital information holds for patients with various Myofascial Pain Syndromes and successful professional treatment in therapy.
Carro L.P., Hernando M.F., Cerezal L., Navarro I.S., Fernandez A.A., Castillo A.O. Deep gluteal space problems: piriformis syndrome, ischiofemoral impingement and sciatic nerve release. Muscles, Ligaments and Tendons Journal, 01 Jul 2016, 6(3):384-396
Fede, C., Pirri, C., Fan, C., Petrelli, L., Guidolin, D., De Caro, R., & Stecco, C. (2021). A Closer Look at the Cellular and Molecular Components of the Deep/Muscular Fasciae. International Journal of Molecular Sciences, Jan 30, 22(3), 1411.
Laurent, T. C., Laurent, U. B., Fraser, J. R. (1996). The structure and function of hyaluronan: An overview. Immunology & Cell Biology, Apr, 74(2), A1-7.
Matteini, P., Dei, L., Carretti, E., Volpi, N., Goti, A., & Pini, R. (2009). Structural Behavior of Highly Concentrated Hyaluronan. Biomacromolecules, Jun 8, 10(6):1516-1522.
Meyer, K., & Palmer, J. W. (1934). The Polysaccharide of the Vitreous Humor. Journal of Biological Chemistry, December, 107(3), 629-634.
Pratt, R. L. (2021). Hyaluronan and the Fascial Frontier. International Journal of Molecular Sciences, Jun 25, 22(13), 6845.
Stecco, C., Stern, R., Porzionato, A., Macchi, V., Masiero, S., Stecco, A., & De Caro, R. (2011). Hyaluronan within fascia in the etiology of myofascial pain. Surgical and Radiologic Anatomy, December, 33(10), 891–6.
ABOUT THE AUTHOR
Dr. Turchaninov graduated with honors from the Odessa Medical School in Ukraine in 1982. He was admitted to the residency program of the Kiev Scientific Institute of Orthopedy and Rehabilitation, which he completed in 1985.
From 1986 to 1992, he worked as a supervisor of the rehabilitation program for the Ukrainian Ministry of Public Health and later as a scientific researcher at the Kiev Scientific Institute of Orthopedy and Rehabilitation. During these years, he also worked with the medical team of the relief effort following the Chernobyl nuclear plant disaster.
In 1989, Dr. Turchaninov obtained his Ph.D. in medicine and graduated from the manual therapy and medical massage programs designed for physicians.
In 1992, Dr. Turchaninov was invited to work in rehabilitation centers in New York City and Scottsdale, Arizona, as head of their medical massage program.
Dr. Turchaninov is the author of more than 100 scientific papers and publications in European and American medical and massage journals. He is the author of three major textbooks: Medical Massage, Volumes I and II, and Therapeutic Massage: A Scientific Approach. He lectures in the U.S. and abroad on manual therapy and medical massage and is regularly invited to speak at American and international conferences.
Dr. Turchaninov founded the Science of Massage Institute, which brings clinical science into massage therapy and builds professional bridges between medical and massage communities. Dr. Turchaninov is the Editor in Chief of the Journal of Massage Science.
Dr. Turchaninov lives in Phoenix, Arizona. His interests are literature, art, history, and travel.
Category: Medical Massage
Tags: 2023 Issue #3