by Dr. Ross Turchaninov
In Part I of this article published in Issue #3, 2014 of JMS we discussed the Gate Control Theory of Pain and its clinical applications. Part II published in Issue #4, 2014 of JMS covered the Neuromatrix Theory of Pain and its clinical meanings.
In this final Part III we will put all this information together as one practical approach to efficiently controlling the pain analyzing system in the therapy room. It will be more understandable if we will logically arrange information we discussed in the previous articles using the example of a hypothetical medical massage session of a patient with right side lower back pain due to acute spasm in the lumbar erectors.
FIRST STAGE:
INITIAL INTERACTION WITH PATIENT AND CLINICAL INTERVIEW
Application of the Neuromatrix Theory
Control of the pain analyzing system starts long before the actual treatment begins. From the very beginning the patient must feel in the right place where his or her issues are going to be answered correctly and the therapist is going to do whatever it takes to help. If the office, therapy room and practitioner don’t create such assurance, the therapist is already in the position of losing the battle with the pain analyzing system.
A majority of waiting and therapy rooms in massage establishments are trying to create the sensation of tranquility and a stress-free environment and no one disputes this value. However, every massage business is doing exactly the same thing from a sitting Buddha statue to a water fountain and candle light. The more the therapist deals with medical issues in his or her practice the more sophisticated the office should look. Your goal is to create the sense of a highly skilled professional who is dedicated to helping people with different pathologies.
From the perspective of our patient with acute lower back pain who has difficulty getting to the office, seeing only a Buddha statue will not encourage much confidence. Let Buddha project a sense of tranquility in the waiting room, but give the new patient some essence before he or she even sees you. Here are examples:
1. Be sure the waiting room introduces you in correct way. It’s supposed to be well maintained.
2. Put your and your colleagues’ pictures on the wall with a short bio emphasizing your educational and clinical experience. You may also use flyers, but pictures are more effective.
3. Place in the waiting room some educational materials about the most frequent conditions you encounter. It can be in the form of posters as well.
4. Ask the patients you helped to describe their experiences in testimonials with their names. Download these files into a large size digital photo frame which can be viewed from different parts of the waiting room and let the testimonials rotate on the screen.
You aren’t doing this for your own vanity. By employing these and similar psychological techniques you start to use principles of the Neuromatrix Theory of Pain and control the central component of the pain analyzing system even before you see the patient for the first time.
The Clinical Interview is the next critical step in the control of the pain analyzing system. Besides providing the therapist with priceless clinical information, it allows you to establish trust in the treatment and in the therapist. Without this important component the control of the pain analyzing system will be a great challenge for the therapist since he or she lost the ‘placebo effect’ as a healing factor.
The Placebo Effect
Generally speaking, the placebo effect is the ability of any medication or treatment procedure to exhibit clinical results simply because the patient believes that it will work. Until recently we discarded the placebo effect as a necessary evil and used it to evaluate the effectiveness of a new drug or procedure. Recently this situation has changed since more and more researchers look at the placebo effect as an important healing factor since it illustrates the healing power of the brain.
“Placebo triggers the body’s natural response, which is defined here as the healing force of nature.”
Zajicek, (1995)
Some modern studies have illustrated that the placebo effect may be responsible for up to 50% of medications’ clinical outcomes (Kam-Hansen et al., 2014) compared to 25-35% as it was thought before.
There are different theories which explain how placebo works and how it can be used clinically. One of the theories directly touches the subject of this article. Dr. W. A. Brown, a psychiatrist at Brown University, emphasized that (Talbot 2000):
“There is certainly data that suggest that just being in the healing situation (bold by JMS) accomplishes something.”
and
“Thus the process of administering therapy is the key factor of the placebo effect. The touching, the caring, the attention, and other interpersonal communication that is part of the controlled study process (or the therapeutic setting), along with the hopefulness and encouragement provided by the practitioner, affect the mood, expectations, and beliefs of the patient, which in turn triggers physical changes such as the release of endorphins, catecholamines, cortisol, or adrenaline.”
Thus being already in the correct environment triggers the healing power of the placebo effect. The therapist uses the placebo effect as an introduction to the actual treatment but not as treatment strategy.
The practitioner must skillfully use the healing power of the brain as an integrative tool of the therapy session and the first step in it is a correctly conducted clinical interview. We published a detailed article on this subject titled “Science of Clinical Interview” in Issue #1, 2012 of JMS. We highly recommend it to therapists.
Professional Communication
Another important issue the therapist must remember is the necessity to explain to patients to the best of therapist’s ability what they are suffering from. It also gives the patient a sense of being with the right practitioner.
As it was shown by Moseley (2004) in a study of 121 participants with chronic lower back pain “…one-to-one education session with researcher about either lumbar spine physiology or pain physiology” improved the clinical picture of chronic lower back pain in the form of increased lumbar flexion and improved Straight Leg Raise Test.
Thus, a professional environment, a correctly conducted clinical interview, knowledge of the subject, the ability to answer the patient’s questions and explaining the nature of the pathology, treatment protocol, its goals and expected outcomes – all these components of the First Stage are designed to elicit central control over the pain analyzing system and this process is under the umbrella of the Neuromatrix Theory of Pain which we discussed in Part II of this article in the Issue #4, 2014 of JMS.
SECOND STAGE:
TREATMENT PROTOCOL
Application Of The Gate Control Theory Of The Pain
After the therapist successfully finishes the first stage of pain control he or she must formulate a treatment routine and implement it. The second stage is governed by the Gate Control Theory of Pain and during this stage the therapist addresses peripheral and central components of the pain at the same time.
Please remember: Pain is ghost! Don’t chase pain – control it!
PAIN IS A GHOST
If our hypothetical patient with lower back pain correlated the onset of his symptoms with acute trauma, the therapist faces a straightforward treatment choice, which is the application of MEDICAL MASSAGE PROTOCOL for the lower back pain associated with trauma and tension in the Lumbar Erectors. The first goal of this protocol will be control of the pain analyzing system.
If the patient didn’t have acute trauma the therapist is presented with two possible scenarios:
1. The pain is a result of chronic, repetitive overload.
In this scenario the same Lumbar Erectors MEDICAL MASSAGE PROTOCOL should be used.
2. Pain is neurological in nature.
Readers will be surprised by how many patients with lower back pain have this mechanism as a main cause of their pain without therapists realized that. In such case the spinal nerve(s) which is supposed to innervate lumbar erectors slightly irritated by the intervertebral disk, ossificated ligaments, bone spurs or tension in lumbar rotators.
In all these scenarios the application of the Lumbar Erectors protocol is useless since a completely different treatment strategy must be implemented. Thus if the therapist makes a mistake during clinical evaluation he or she will chase the ghost of pain.
DON’T CHASE THE PAIN BUT CONTROL IT
The therapist made the correct treatment choice and now it is time to start therapy of our hypothetical patient with Lower Back Pain. Again, the control of the pain analyzing system is the first critical component. All other issues like postural imbalance, secondary symptoms in the form of pelvis rotation or thorax twist are completely irrelevant at this point and they continue to be irrelevant until the therapist has complete control over the pain analyzing system.
It doesn’t matter what you were taught in school or by different educators. Control of the pain analyzing system is the first necessary step. The rest of the treatment options will follow later. However, in many cases these treatments may not be needed since the body has a great ability to balance itself as soon as pain isn’t a factor anymore. How do you control the pain analyzing system efficiently? The therapist doesn’t have many tools so this is why every tool he or she has is so precious, as is their correct arrangement.
If a therapist thinks he or she is able to overplay the patient’s pain analyzing system by exceeding its threshold with harmful pressure, he or she will be defeated since the patient’s brain is smarter than any courses and certifications the therapist has accumulated. Please remember that the troops and guards the brain employs are more sophisticated than your system of beliefs. Thus the only way to control the patient’s pain analyzing system is to mislead it! Instead of trying to take it down with a frontal assault, try to find a little back door. Here are the tools for cheating the patient’s brain, using principles of Gate Control and the Neuromatrix Theories of Pain:
1. Inhibitory Regime of Massage
2. Permanent Electric Vibration
3. Work on a Layer by Layer Basis
Our hypothetical patient with lower back pain due to spasm in the lumbar erectors is on the table. As we discussed above, before any special medical massage tools are used – myofascial release, cross fiber frictions, various stretching and mobilization – the therapist has to control the pain analyzing system. The best way to do it is with an inhibitory regime of massage therapy applied within areas the patient feels pain (Ivanichev, 1990; Goldberg et al., 1992).
The inhibitory regime requires the application of identical massage strokes applied in the same direction with the same speed and pressure. The practitioner should mostly use kneading or a combination of effleurage (30%) and kneading (70%). Direct all strokes along the lymph and venous drainage. Usually 3-5 minutes of massage in inhibitory regime is enough to decrease protective muscle tension and desensitize segments of the spinal cord responsible for the innervation of the affected area.
Let’s discuss the physiological mechanism behind the inhibitory treatment with help of
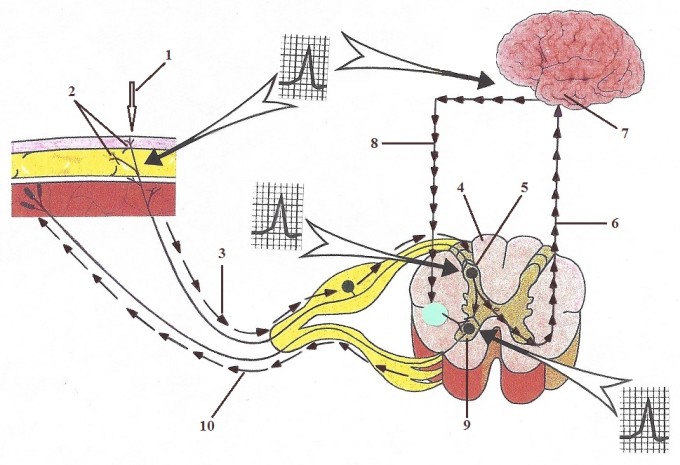
Fig. 1. Inhibitory regime of massage therapy. Beginning of the treatment
1 – initial light touch
2 – peripheral receptors in the soft tissue
3 – ascending sensory flow of action potentials to the spinal cord
4 – segment of the spinal cord responsible for the innervation of the massaged area
5 – sensory ‘computer’ in the posterior horns of the spinal cord
6 – sensory ascending flow to the brain
7 – upper motor center
8 – descending motor control from the upper motor center to reinforce the action of lower motor
center
9 – lower motor centers in the anterior horns of the spinal cord
10 – motor flow back to the massaged area
Large arrows indicate areas where the action potentials are generated
The patient with any type of pain is on the table and he is comfortable. However, as soon as the therapist even lightly touches the area where patient feels pain (see Fig. 1, ‘1’), all of this will immediately change. The peripheral receptors (see Fig. 1, ‘2’), in the area of pain already have a low threshold of activation and their even mild additional stimulation will create massive sensory input (see Fig. 1, ‘3’), to the sensory computer located in the posterior horns of the spinal cord (see Fig. 1, ‘5’). The activation of posterior horns triggers stimulation of the lower motor centers located in the anterior horns of the spinal cord (see Fig. 1, ‘9’), which in turn trigger massive motor response (see Fig. 1, ‘10’), to the areas the therapist lightly touched. It immediately increases the protective muscle tension.
Also, from posterior horns the sensory flow (see Fig. 1, ‘6’), speeds up to the upper motor centers in the cortex (Fig. 1, ‘7’). When the upper motor centers are activated, additional descending motor flow (see Fig. 1, ‘8’), is conducted via the lateral corticospinal and rubrospinal tracts (Fig. 1, ‘8’) to the same lower motor centers which are located in the anterior horns of the spinal cord.
Thus the lower motor centers are simultaneously activated from the sensory computer located in the same segment of the spinal cord and additionally by upper motor centers. Such joined stimulation of lower motor centers enhances the descending flow of motor impulses to the soft tissues the therapist touched. Thus the first patient reaction to the light touch of the painful area is an uncontrollable body defense reaction to the therapist’s intrusion.
The inhibitory regime of massage therapy when applied correctly changes the situation quickly in the therapist’s favor (see Fig. 2).
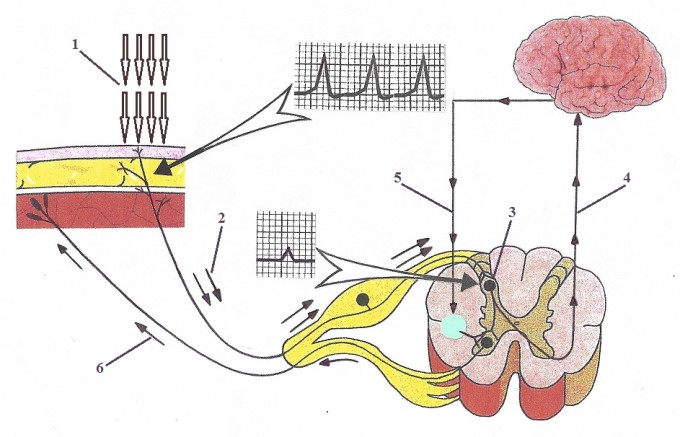
Fig. 2. Inhibitory regime of massage therapy
1 – repetitive massage strokes
2 – massive flow of sensory stimuli to the spinal cord
3 – ‘sensory’ computer in the posterior horns of the spinal cord
4 – diminished sensory influx to the brain
5 – decreased stimulating flow from the upper to lower motor center
6 – decreased flow of motor stimuli to the massaged area
If the practitioner works in the inhibitory regime (Fig. 2, ‘1’), i.e., with the same techniques, on the same area, with the same pressure for a few minutes – the ‘sensory computer’ in the posterior horns of the spinal cord (Fig. 2, ‘3’), is inhibited by the massive, continuous flow of information from the peripheral receptors (Fig. 2, ‘2’). Since these stimuli didn’t alarm the pain analyzing system, the ‘sensory computer’ will close the gates in the posterior horns of the spinal cord, refusing to accept the influx of sensory information as dangerous. As a result, the number of motor commands to the massaged area decreases (Fig. 2, ‘6’), and protective muscle tension will partly melt away. This process reinforced by the decrease of stimulating motor control from the upper motor centers (Fig. 2, ‘5’), because the sensory influx to the brain diminishes (Fig. 2, ‘4’), as a result of ‘gates’ closing.
Later the peripheral receptors will reach their own adaptation level and the production of sensory
stimuli to the spinal cord will also decrease and it additionally helps with a decrease in protective muscle tension (Turin, 1992).
The inhibitory regime of massage treatment significantly suppresses initial pain. A massive afferent flow of sensory impulses generated by massage strokes helps to keep the “gates” in the spinal cord in the closed or partly open position, blocking the conductance of noxious stimuli to the central nervous system, followed by the suppression of pain formation by the brain. This effect of inhibitory treatment can also be successfully used for pain reduction on patients following surgery, or for those with cancer, causalgia, etc.
Marin, et al. (1991) analyzed the effect of massage treatment on 116 patients following a thoracotomy. The massage therapy in the inhibitory regime started on the first day after surgery and continued for eight days. The analgesic effect of massage therapy was estimated using a Visual Analog Scale. The degree of pain suppression reported by all patients after massage treatment was statistically significant enough to consider the massage therapy as an important clinical tool in controlling the pain analyzing system.
Another tool to control the pain analyzing system in sensitive areas is permanent, electric vibration. Based on their own experimental studies and a classic study conducted by Dr. Zotterman in 1939, Prof. Mezlack and Prof. Wall, fathers of the Gate Control Theory of Pain, proved that the application of permanent electric vibration has a dual therapeutic effect. It desensitizes the nociceptors and, more importantly, it closes the ‘gates’ of the sensory computer in the spinal cord and inhibits the acceptance of the noxious stimuli on the level of the central nervous system. The last analgesic effect is much more profound and long lasting. It blocks the peripheral component of the pain analyzing system on the level of the spinal cord.
Wall and Crowly-Dillan, (1960) in a series of experiments showed that vibration inhibits all types of nociceptors and proprioceptors (i.e., touch, pressure, temperature). The authors also pointed out the central inhibition of proprioceptors, especially nociceptors. The authors considered two possible mechanisms of central inhibition of pain by the vibratory stimuli: blocking and reduction of sensory impulses in size and number, and the increasing of the threshold of nervous cells activation in the CNS. Thus, the massage practitioner should use permanent vibration in all sensitive areas. It will set the gates in a more closed position and help to control pain stimuli during the treatment.
It is better to apply fixed, permanent vibration to the painful areas after the inhibitory regime of massage therapy. For the vibration to inhibit the pain analyzing system, the massager must generate true vibration rather than vibration as a result of percussion. The frequency of oscillation must be at least 60 Hz and the contact area of the machine must be semi-soft or it can be applied through a towel.
After putting the massager in place, don’t move it. To inhibit, the vibration should be applied in a fixed regime. If the therapist moves or applies and withdraws and again re-applies the massager, the treatment will have the opposite effect. It will stimulate the peripheral receptors and CNS, decreasing the effectiveness of the inhibitory regime of massage therapy the therapist used first.
WORK WITH SOFT TISSUES ON A LAYER BY LAYER BASIS
Let’s look at Fig. 3, which illustrates the basic arrangement of the soft tissues in the human body.
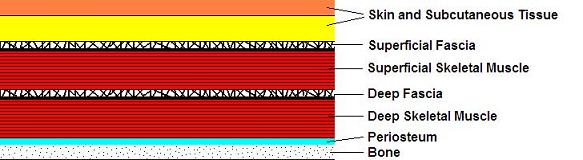
Fig. 3. Basic soft tissue arrangement
This basic arrangement is identical and only the possible variations are one or two extra layers of skeletal muscles separated by fascia. For example, in our hypothetical case the lower back area will have four layers of skeletal muscles instead of two shown in Fig. 3. These levels are: latissimus dorsi-fascia-lumbar erectors-fascia- quadratus lumborum-fascia-iliopsoas.
If we all agree with this arrangement it becomes obvious that each layer of the soft tissues has a unique histological structure, unique anatomical arrangement and unique functions. What muscles can do, the skin is unable to do and vice versa. Because of the layer by layer soft tissue arrangement, nociceptors in the soft tissues do not spread equally and even the nature of peripheral receptors is different in each layer. For example, one will never find muscle spindle receptors in the skin or fascia, while Pacinian corpuscles which are abandoned in the skin have much less presence in the fascia.
All of this requires the layer by layer approach to the soft tissue treatment in general, but it becomes even more important when the therapist tries to control the pain analyzing system.
What does it mean to work on layer by layer basis? For example, Myofascial Release is an excellent tool to address different layers of fascia but it has limited clinical potential while addressing the skin. At the same time, Mobile Cupping or superficial friction specifically targets the skin. Thus to work on a layer by layer basis means the therapist has to have a large professional tool box to match the layer of the soft tissues with corresponding Medical Massage technique.
Of course, there are more universal Medical Massage methods, e.g., Neuromuscular Therapy or Segment-Reflex Massage, but they also miss important components of the therapy like Periostal Massage to address periosteum or Lymph Drainage Massage. Unfortunately for patients, the majority of therapists lack such a comprehensive vision of somatic rehabilitation because they lock themselves within a box of one or two techniques they learn without the ability to integrate various techniques in one perfect Medical Massage session.
To conclude, during the second stage of treatment the main accent is on the principles of the Gate Control Theory of the Pain while the principles of Neuromatrix Theory play a supportive role.
THIRD STAGE:
THE PATIENT’S HOMEWORK
Application Of The Neuromatrix Theory Of Pain
The session is finished and the patient is ready to leave the therapy room. If the patient doesn’t feel the therapist’s ‘invisible presence’ between sessions, the therapist failed to recruit the patient as a critical component of the therapy. Thus, the therapist shouldn’t let the patient just walk away and come back for the next session. Everything that was done and achieved during the session must be supported by the patient at home between the sessions. First of all, it greatly reduces the number of needed sessions and secondly, it maintains the foundation for the therapist to push forward during future treatments.
Also, the patient’s homework has another great benefit in that it helps the therapist to additionally control the pain analyzing system. By giving the patient a set of home stretches or other recommendations, it actively engages them into the treatment process. One of the great tools we use in our clinic is little diary we ask our patients to keep between the sessions. Ask them to write down when and what they do during the day to support the results of the previous session. Are there any symptoms and new changes they observed in their bodies? What was the level of pain during the day, etc.
Be sure to carefully read these notes before the next session and thank the patient several times for doing such a great and important job. You will be surprised to what extent patients will go with your recommendations and how much empowering the patient gives you additional leverage to help them quickly and efficiently. During the third stage you control the pain analyzing system using principles of Neuromatrix Theory.
CONCLUSION
In our clinic we regularly see patients who were treated in chiropractic, physical therapy or massage offices where the “No pain, No gain” approach was used. In cases of somatic pathologies, this is no less than a completely outrageous habit of professional incompetence. It is the therapist’s professional duty to control the pain analyzing system first, before any other stabilization, stretching, postural alternation, etc. approaches are used. This three part article tried to illustrate this important first step in the treatment process.
REFERENCES
Ivanichev, G.A. Painful Muscular Hypertonus and Trigger Points. Kazan Medical University, Kazan, 1990
Golberg, J., Sullivan, S.J., Seaborne, D. E. The Effect of Two Intensities of Massage on H-Reflex Amplitude. Phys. Ther., 72(6), June, 449-457, 1992
Kam-Hansen S, Jakubowski M, Kelley JM, Kirsch I, Hoaglin DC, Kaptchuk TJ, Burstein R. Altered placebo and drug labeling changes the outcome of episodic migraine attacks. Sci Transl Med. 2014 Jan 8;6(218):218ra5.
Marin, I, Lepresle, C., Mechet, M.A., Debesse, B.: Postoperative Pain after Thoracotomy. A Study of 116 patients. Rev. Mal. Respir., 8(2): 213-218, 1991.
Mezlack, R., Wall, P. Pain Mechanism: A New Theory. Science, 150 (Nov): 971-979, 1956
Moseley G.L. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain 2004;8:39–45
Talbot, M. The Placebo Prescription, New York Times Magazine, January 9, 2000.
Turin, A.M.: Traditional and Nontraditional Massage. “Iscusstvo-CPB”, St. Petersburg, 1992.
Wall, P.D., Crowly-Dillon, J .R.: Pain, Itch and Vibration. A.MA. Arch. Neurol., 2: 19-29, 1960.
Zajicek G. EDITORIAL. The placebo effect is the healing force of nature. The Cancer Journal. 1995, March-April 8(2).
Zotterman, Y. Touch, Pain and Tickling: an Electrophysiological Investigation on Cutaneous Sensory Nerves. J. Physiology, 95:1-28, 1939
For Dr. Turchaninov’s biography, please click here.
Category: Medical Massage
Tags: Issue #1 2015
