By Karen Mooney, PhD, LMT, CMMP
This article is contributed by Karen Mooney, LMT, PhD, CMMP. She is our former student and is an exceptionally talented therapist, educator and now massage scientist. We don’t have many PhDs in our profession who earned their degree specifically in the massage therapy field. However, this is not all. Karen’s PhD is the first degree in the USA awarded to a therapist in the Medical Massage field and this is the most exciting news for all of us in SOMI and we hope for all massage therapists.
Here is the opinion of Dr. D. Moss, Chair of the Graduate School of Mind-Body Medicine from Saybrook University expressed about Karen’s PhD dissertation:
“This is one of the best written and best edited dissertations I have ever received for review. Each chapter is well organized and clear. I am just completely impressed and proud of the work you have done. You know me. I usually send back pages of red marks and comments. No student has ever received so little markup the first time a final copy was submitted. This is an excellent study, and must get published.”
Dr. D. Moss
The article you will read below summarizes the result of a study Karen conducted to examine the effect of soft tissue rehabilitation in patients with Fibromyalgia. There is another unique aspect of her work. Instead of testing a single modality or approach, Karen materialized the main point of our vision she also shares – successful somatic rehabilitation as a result of the integration of different modalities. It is a dead end in our profession if therapists let themselves be pulled into a world where massage therapy is fragmented and Karen’s PhD is a great illustration of how it should be.
R. Turchaninov, Editor in Chief
INTRODUCTION
The purpose of this study is to evaluate an integrative mind-body protocol that has been specifically developed for mitigation of symptoms in Fibromyalgia (FM) patients.
The occurrence of this chronic pain disorder according to The National Fibromyalgia As-sociation:
“affects an estimated 10 million people in the U.S. and an estimated 3-6% of the world population. It is most prevalent in women – 75-90% of the people affected.”
There are no lab tests or imaging techniques that provide conclusive evidence of FM presence in the patient (Fürst, 2007), but rather, assessment depends on symptom severity (Clauw, 2009). The accumulation of research has led to inconsistencies, confusion, and ineffectual treat-ment plans (Häuser, et al., 2010). FM has been notoriously unresponsive to allopathic medical treatments (Adsett, 2007; Simms, 1998).
The etiology remains conjecture and central mechanisms hypothesis (Vierck, 2006) is the dominating concept which concentrates on the central disinhibition, central sensitization, and the dysfunctional response of the hypothalamus–pituitary–adrenal axis (HPA):
“Pain signaling is a complex interaction between ascending and descending path-ways between the spinal cord and brain.” (Krypel, 2009, p. 7)
These studies shed light on the whole body response to pain for the FM patient, but make no claim to define the etiology of patho-physiological events associated with FM.
Some researchers look beyond the central nervous system’s changes and imbalances in the modulating pathways (Yunus et al., 1989; Staud, 2004, 2006; Turchaninov, 2006; Vierck, 2006). These authors acknowledge the bidirectional relationship (Fig. 1) of hypersensitive nociception input and heightened central pain processing but do not believe it originates in the CNS. The focus of this group turned to a peripheral root source for the hyperalgesia. Figure 1 summarizes the bidirec-tional distribution of clinical pain and hypersensitivity of FM patients.
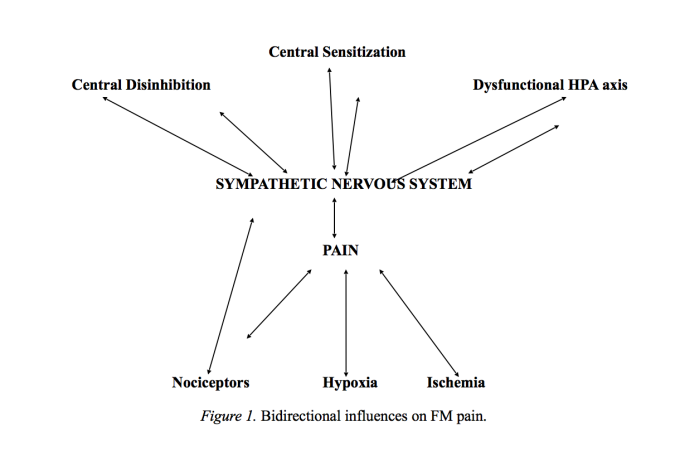
Fig. 1. Bidirectional influences on FM pain.
The role of peripheral mechanisms in the changes of the CNS is subject to much conjecture. Some progress in understanding the relationship is made with the factors identified by Vierck (2006) which acknowledged that until a source is recognized in the CNS, peripheral mechanisms must be considered.
In the systematic review of this study, (Mooney, 2015) muscle pathology has been shown to have a clear origin and progression (Popelansky & Ivanichev, 1984; Yunus et al., 1989; Sprott et al., 2004) that explains many of the events leading to the hyperalgesia in the soft tissues and, ultimately, the changes in the central nervous system, viscera, emotions, and behaviors associated with FM. However the initial trigger associated with the onset of muscle pathology associated with FM occurs following physical or emotional trauma or stress.
The development and progression of muscle abnormalities offers an explanation for the peripheral mechanisms observed in patients with FM (Mooney, 2015). These events appear to be provoked by a physical and/or emotional impact (Goldenberg, 1999; Ogden et al., 2006; Scaer, 2007; Staud, 2007), chronic overuse of a muscle group (Popelansky & Ivanichev, 1984), or a his-tory of accumulated distress. These circumstances set the stage for an unresolved stress response in the body or somatization and muscle pathology resulting in ischemia and hypoxia (Levine, 1996; Ogden et al., 2006; Popelansky & Ivanichev, 1984; Scaer, 2007).
STANDARD TREATMENT STRATEGIES
Since the theory of central mechanisms of FM currently prevails, the array of medications used to address symptoms of FM includes antidepressants, opioids, nonsteroidal anti-inflamma-tory (NSAIDS) drugs, muscle relaxants, anticonvulsants, sedatives, analgesics, and hypnotic agents (Han et al., 2011).
The overall failure of pharmacological intervention and its erratic results has caused some authors to suggest other forms of therapy with or without the drug treatments (Fürst, 2007; Ja-han, et al., 2012; Littlejohn & Walker, 2002; Staud, 2010).
STUDY DESIGN
The two major components of the protocol were combined in this research – Medical Massage and Gentle Movement Therapy. They were chosen to address the symptoms, provide a proactive treatment plan, and create a supportive, motivating environment while addressing:
1. The somatic expression of trauma
2. The hypertonicity in muscles and formation of tender points
3. Low grade ischemia
4. Insufficient drainage
5. The limiting influence of adaptive movement patterns
6. The cognitive and pathological influences on the mind and body of the patient with FM
7. Formation of pain perception by the brain
Six individuals were asked to complete interviews, questionnaires, personal journals, and assist with progress notes. The participants previously diagnosed with FM by an attending physi-cian using the American College of Rheumatology preliminary diagnostic criteria for FM (Wolfe, et al., 2010) were randomly selected from a large group of volunteers providing the criti-cal cases.
A copy of the diagnostic criteria was given to each volunteer and a suggestion was made to all volunteers to consult with their attending physician. Each person came into the study at a different stage of FM and each was expected to respond differently to the study’s intervention program. Volunteers presently taking an opioid medication or ketamine in any form were not in-cluded. Taking other medications or supplements was acceptable. Participants were asked not to add any new medications or treatments during the study. Also, patients under active chiropractic care were excluded.
The design of this study utilized a mixed method approach including a multiple case study (qualitative) and pre- and post-intervention measurements (or repeated measures) for quan-titative data. The study relied on the experience of the individual case to answer the questions (intrinsic), but the study also served as an instrument to further understanding of FM (Stake, 1995). Table 1 is a summary of data collecting instruments, time each was used, and reasons for selection.
| Intake Interview | Before treatment protocol or the first week preceding the study | Qualitative
Medical history Symptoms Medications Interventions Lifestyle Onset of problem Baseline |
| Personal Journaling | First week and continuing throughout the study | Qualitative
Subjective self-report of pertinent daily behaviors, symptoms, changes, needs |
| Progress Notes | Sequential with intervention | Qualitative
Therapist & participant report |
| Revised Fibromyalgia Impact Questionnaire (FIQR) | First week preceding study;
Within 5 days following study |
Quantitative
Current Evaluation: physical functioning socio-cultural impact, ability to perform mental tasks |
| The Brief Pain Inventory
( BPI) |
First week preceding study;
Within 5 days following study |
Quantitative
Self-report of the intensity and the reactive dimension of pain |
| Patient Global Impression of Change (PGIC) | Within 5 days following study | Quantitative
Overall improvement in pain and symptoms |
| Exit interview | Within 5 days following study | Qualitative/Quantitative
retake assessments subjective impressions |
COMPONENTS OF THE PROTOCOL
The first phase of the intervention protocol consists of twelve, 40 to 60 minute treatments of Medical Massage. To elicit clinical changes for the participants with FM, the protocol inter-vention uses techniques of the Medical Massage modality to address the peripheral mechanisms with expectation that normalization function of soft tissues will respectfully normalize function of CNS affected by chronic activation of nociceptors.
The role of the MEDICAL MASSAGE PROTOCOL in this effort is essential to:
* release the somatic manifestations
* reset the balance between sympathetic and parasympathetic divisions of autonomic nervous system
* treat hypertonically changed muscles eliminating tender points
* decrease intensity of pain perception
* allow the participant to experience his or her own body in a positive way
* restore normal blood flow and drainage thorough the affected soft tissue
* validate the participant’s perception of the state of the body while creating a compassionate, safe, and nurturing environment
* address the chronic, persistent psychological aspects of FM
First phase: Medical Massage
Each session began with the participant lying prone in anatomical position, using a face cradle and a foot bolster of comfortable size. Attention to comfort, temperature, position, sounds, present pain levels, and areas of hyperalgesia was paramount. All factors for each individual and each session were recorded in treatment notes.
A discussion of pressure and discomfort alerted the participant to be vigilant and control these factors throughout the session. Feedback is imperative to enable the practitioner to meet the goals of the treatment but also for the patient to have expression and control of personal needs.
Described here are the initial 2 sessions of therapeutic massage in the inhibitory regime (Turchaninov, 2006) applied to the upper torso only. To avoid potential autonomic reactions like nausea, headaches and flu-like symptoms following massage reported by many FM patients, this method was selected to consider the years of accumulated metabolic ‘waste’ resulting from the low ischemia and pathologically changed drainage in the affected soft tissues.
These initial sessions establish rapport, trust in the process, patient control, and enable the therapist to assess the tolerance and needs of each person. In a sense these initial sessions formed the skeleton of the therapy with further addition of specific Medical Massage techniques into each treatment session while addressing each of the tender points associated with personal pattern of FM distribution in each patient.
The practitioner should be aware that the goals listed previously apply to each session. The pressure of all strokes must be comfortable for the patient and below the personal pain threshold. With every session this threshold was reassessed for each contact area. Please refer to Therapeutic Massage. A Scientific Approach (Turchaninov, 2000) for the definition and proper technique of each stroke used during the therapy.
Step 1: Addressing the whole back from sacrum to cervical and across shoulders, apply long gentle, bi manual effleurage strokes. This allows the practitioner to activate the parasympathetic response, initiate a state of relaxation, and assess the contact areas for pain thresholds. Using full hand effleurage strokes, cover the entire back from sacrum to cervical for several minutes The strokes should be consistent, smooth, and non-aggressive. It is important to next ad-dress the paravertebral muscles on each side with the Big Fold stroke. Begin on the most affected side with the Big Fold technique first then move to the least affected side and apply the same.
Step 2: Remaining on the least affected side and working across the body, apply the stronger effleurage strokes to the neck and shoulder from medial to lateral in the direction of drainage. Continuing in the inhibitory regime, add a full hand repetitive friction moving down the neck, across and to the point of the shoulder. Adjust pressure to what is comfortable, maintain contact, and follow with effleurage. The practitioner then physically moves to the least affected side to continue addressing that shoulder, scapula and upper thoracic area with general effleurage in the direction of drainage and non-specific friction strokes. While maintaining contact, return to the other side and work across the body again with raking effleurage and friction from thoracic to lumbar between ribs.
Step 3: Effleurage and friction through the lumbar and sacral area, addressing the soft tis-sue insertions. Move up the back again with the Big Fold. Move again to the same side and effleurage the entire side of the back. Big Fold the paravertebrals on the opposite side then repeat steps 1 through 3 on that side of the back.
Step 4: Finish the posterior by addressing the whole back again from sacrum to cervical with various effleurage strokes. The patient often comments that this feels as if the parts are re-connected to the whole.
Step 5: Turn to supine position. Apply effleurage and friction to arms, shoulders, neck, and complete gentle facial massage in the direction of the drainage to the anterior neck.
Second phase: Slow Movements
The second component in the protocol is an 8-session program of structured movements. The movement class is a group activity, meeting for 1 hour a week for six sessions. The move-ment group meets simultaneously with the Medical Massage interventions. In a clinical setting the movement class would include other mind/body interventions such as guided imagery and visualization.
The formation of chronic hypertonic muscle pathology eventually results in new muscle patterns which limit range of motion and normal function (Hanna, 1988). Acknowledging the in-fluence of somatization of stress or trauma and musculoskeletal dysfunctions in cases of FM sup-ports the clinical relevance of the movement portion of the protocol.
Exercise and aerobics have been studied and used with FM patients, but the focus has not been to restructure the cortical maps, release the trauma, or to alter the pathological progression (Häuser, et al., 2010). To restructure the brain map into a more productive movement pattern, it is necessary to expand and refine attention through slow, exact movements while focusing on the sensation of the movement (Feldenkrais, 1977; Daly & Ruff, 2007).
The slow repetitive movement rebalance of agonist/antagonist muscles, decreases efforts of muscle synergists, and reduces muscle hypertonicity. For example, as the patient slowly and methodically moves the legs in a precise pattern, the threshold of the muscle spindle receptors are reset but in a careful, nurturing manner. The patient is then able to adjust the movement to the new threshold and increase the range of motion without creating any muscle tension. As the range of motion increases, with cautious adjustments, the muscle tension is reduced and so is the associated, devastating ischemia (Feldenkrais, 1977; Turchaninov, 2006).
Movement goals include:
* awareness and release of restrictive patterns
* awareness and release of pain patterns
* providing a proactive response to stress
* reconnecting motor cortex and muscle spindle receptors on the normal, physiological range
* reorganizing the cortical maps (Hanna, 1990-1991; Mahncke, et al., 2006)
* awareness of personal somatic responses to stress/trauma, and reducing muscle tension
RESULTS
For the complete statistical analysis results of the study please click here. The information presented below is a shortened version of the original study results.
Quantitative Data and Analysis
1. Revised Fibromyalgia Impact Questionnaire (FIQR)
According to results of Revised Fibromyalgia Impact Questionnaire the participants in this study showed a statistically significant difference between the scores at the base measure-ment and the end scores post-intervention with high practical significance of this change.
The statistical results suggest all participants experienced relief from the FM symptoms that limited their normal daily activity and each participant’s ability to function in everyday tasks was enhanced.
The total FIQR demonstrates significant difference between the pre-intervention total (T) score (M = 56.50, SD=14.00) and the post-intervention total score (M = 39.66, SD = 14.14); t (5) = 8.68, p < .001. The Cohen’s d effect size value (d = 1.20) suggested a high practical signifi-cance.
2. Brief Pain Inventory (BPI)
The BPI is used to measure the severity and interference of pain in everyday life. For the participants in this study there was a statistically significant difference between the scores at the base measurement (M = 6.00, SD = 1.90) and at the end measurement (M = 4.17, SD = 1.60); t (5) = 2.60, p = .048. Further, the Cohen’s effect size value (d = 0.96) suggested a high practical significance.
3. Patients’ Global Impression of Change (PGIC)
The PGIC was administered post-intervention providing the participants an opportunity to report any clinical changes. Hurst and Bolton (2004) outlined and noted on the PGIC question-naire the interpretation of this subjective outcome measurement:
* A significant, favorable change is a score of 5–7
* No significant change is a 1–4 response
Also
* A 2-point change indicates significant improvement from their last reported score.
Five participants in our study indicated score 6 while one indicated score 5. Also four of the participants indicated a 2-point change since the beginning of the intervention.
Qualitative Data and Analysis
For the qualitative inquiry in this mixed method research a case study approach provided an in depth understanding of the experience of each participant. Common themes that related to the research question, “How efficacious is a specific theory-based approach, including Medical
Massage and movement therapy, in reducing the symptoms of patients with FM?” added another dimension to the quantitative results. The focus on key issues or themes began within each case followed by a thematic cross-case analysis.
Each participant reported some changes in at least one area of her life. For most it was a reduction in pain, and for some, it was a renewal of sense of self. It seemed to them that any pos-itive change gave them more hope and power, therefore increasing the quality of life.
CONCLUSION
The results of this theory-based protocol for the treatment of FM, including Medical Mas-sage and a Gentle Movement Therapy, showed a statistically significant effect on the mitigation of symptoms for the participants (N = 6) with FM. It is important to reiterate that the protocol evaluated in this study is based on the theory that muscle pathology is a key peripheral mecha-nism, and that trauma plays a critical role.
Although the theory of FM’s central origin currently prevails and there is an abundance of evidence for central processes being affected in FM, the importance of certain peripheral mechanisms has been recognized. Vierck (2006) credits “abnormal peripheral input(s) for devel-opment and maintenance of this condition (FM)” (p. 242), which necessitates a better under-standing of the mechanisms to develop and document adequate therapies.
The statistical results provided preliminary evidence that the protocol may be effectual in improving functional deficits and symptoms of FM. The general improvements noted in the sta-tistical findings of the study included a decrease in pain and muscle tension; less depression and anxiety; and an increased ability to function, set goals and limits.
The qualitative summary of each theme reflected that although the time allowed for this study was limited, participants experienced a substantial reduction in pain and therefore an in-crease in the QoL One participant made the comment that “we cannot heal without addressing both the mind and the body parts of this illness” (JK). We might clinically transfer this infor-mation to other treatment plans for patients with FM.
This study also may be a springboard to further investigation of the progression of muscle pathology discussed here as the “abnormal peripheral input(s) for development and maintenance of this condition (FM)” (Vierck, 2006, p. 242).
REFERENCES
1. Adsett, A. (2007). Somatization disorders [Review of the book Treating somatization: A cog-nitive-behavior approach by R. L. Woolfolk & L. A. Allen]. Canadian Journal of Psychiatry, 52(10), 690.
2. Bennett, R. M., Friend, R., Jones, K. D., Ward, R., Han, B. K., & Ross, R. L. (2009). The Re-vised Fibromyalgia Impact Questionnaire (FIQR): Validation and psychometric properties. Ar-thritis Research & Therapy, 11(4), R120.
3. Boomershine, C. S. (2012). A comprehensive evaluation of standardized assessment tools in the diagnosis of fibromyalgia and in the assessment of fibromyalgia severity. Pain Research and Treatment, 2012, Article ID 653714. Retrieved from http://www.hindawi.com/journals/prt/
4. Buskila, D., & Cohen, H. (2007). Comorbidity of fibromyalgia and psychiatric disorders. Cur-rent Pain and Headache Reports, 11(5), 333–338.
5. Choy, E., Perrot, S., Leon, T., Kaplan, J., Petersel, D., Ginovker, A., & Kramer, E. (2010). A patient survey of the impact of fibromyalgia and the journey to diagnosis. BMC Health Services Research, 10(1), 102.
6. Clauw, D. J. (2009). Fibromyalgia: An overview. The American Journal of Medicine, 122(12, Suppl.), S3–S13l.
7. Daly, J. J., & Ruff, R. L. (2007). Construction of efficacious gait and upper limb functional interventions based on plasticity evidence and model-based measures for stroke patients. Scien-tific World Journal, 7, 2031–2045.
8. Feldenkrais, M. (1977). Awareness through movement. New York, NY: Harper Row.
9. Fürst, G. (2007). Fibromyalgia–a challenge for interdisciplinary management. Wiener Medizinische Wochenschrift [Viennese Medical Weekly, 1946], 157(1–2), 27–33.
10. Goldenberg, D. (1989). Treatment of fibromyalgia syndrome. Rheumatic Disease Clinics of North America, 15, 61–71.
11. Goldenberg, D. L. (1999). Fibromyalgia syndrome a decade later: What we have learned. Ar-chives of International Medicine, 159, 777–785.
12. Han, C., Lee, S.-J., Lee, S.-Y., Seo, H.-J., Wang, S.-M., Park, M.-H., Patkar, A. A.,…Pae, C.-U. (2011). Available therapies and current management of fibromyalgia: Focusing on phar-macological agents. Drugs of Today, 47(7), 539–557.
13. Hanna, T. (1988). Somatics. Reading, MA: Addison-Wesley.
14. Hanna, T. (1990-1991). Clinical somatic education: A new discipline in the field of health care. Somatics, 7(1), 21–38.
15. Harris, R. E., & Clauw, D. J. (2008). Newer treatments for fibromyalgia syndrome. Thera-peutics and Clinical Risk Management, 4(6), 1331–1342.
16. Häuser, W., Thieme, K., & Turk, D. C. (2010). Guidelines on the management of fibromyal-gia syndrome: A systematic review. European Journal of Pain, 14(1), 5–10.
17. Hurst, H., & Bolton, J. (2004). Assessing the clinical significance of changes cores recorded on subjective outcome measures. Journal of Manipulative Physiology and Therapy, 27, 26–35.
18. Jahan, F., Nanji, K., Qidwai, W., & Qasim, R. (2012). Fibromyalgia syndrome: An overview of pathophysiology, diagnosis and management. Oman Medical Journal, 27(3), 192–195.
19. Krypel, L. L. (2009). Fibromyalgia: A review of its pathophysiology and drug treatment. Journal of Pharmacy Practice, 22(1), 6–16. doi:10.1177/0897190008322151
20. Levine, P. (1996). Trauma healing articles. Retrieved from the Foundation for Human En-richment website: http://www.traumahealing.com
21. Leza, J. C. (2003). Fibromyalgia: A challenge for neuroscience. Revista De Neurologia, 36(12), 1165–1175.
22. Littlejohn, G. O., & Walker, J. (2002). A realistic approach to managing patients with fi-bromyalgia. Current Rheumatology Reports, 4(4), 286–292.
23. Lucas, H. J., Brauch, C. M., Settas, L., & Theoharides, T. C. (2006). Fibromyalgia: New con-cepts of pathogenesis and treatment. International Journal of Immunopathology and Pharmacol-ogy, 19(1), 5–10, 91.
24. Mahncke, H. W., Bronstone, A., & Merzenich, M. M. (2006). Brain plasticity and functional losses in the aged: Scientific bases for a novel intervention. Progress in Brain Research, 157, 81–109.
25. Mooney, K. (2015). Exploring the role of peripheral mechanisms: An evaluation of a theory-based approach to reducing symptoms of fibromyalgia (Order No. 3711757). Available from ProQuest Dissertations & Theses Global. (1707928857).
26. National Fibromyalgia Association. (n.d.-b). Prevalence. Retrieved from http://www.fmaware.org/prevalence.html
27. Ogden, P., Minton, K., & Pain, C. (2006). Trauma and the body: A sensorimotor approach to psychotherapy. New York, NY: W.W. Norton.
28. Popelansky, Y. Y., & Ivanichev, G. (1984). Manual therapy of local hypertonuses: PIR method. Kazan, Russia: Kazan University.
29. Rasmussen, L. B., Mikkelsen, K., Haugen, M., Pripp, A. H., & Forre, O. T. (2009). Treat-ment of fibromyalgia at the Maharishi Ayurveda Health Centre in Norway. A six-month follow-up study. Clinical and Experimental Rheumatology, 27(5 Suppl. 56), S46–S50.
30. Rogers, C. R. (1989). Toward a modern approach to values: The valuing process in the mature person. In: H. Kirschenbaum & V. L. Henderson (Eds.), The Carl Rogers reader (pp. 168–185). Boston, MA: Houghton Mifflin.
31. Scaer, R. C. (2007). The body bears the burden (2nd ed).Binghamton, NY: The Haworth Medical Press.
32. Simms, R. W. (1998). Fibromyalgia is not a muscle disorder. American Journal of Science, 315(6), 346–350
33. Sprott, H., Salemi, S., Gay, R., Bradley, L., Alarcon, G., Oh, S., Michel, B., Gay, S. Increased DNA fragmentation and ultrastructural changes in fibromyalgic muscle fibres. Ann Rheum Dis. 2004 Mar; 63(3): 245–251.
34. Stake, R. E. (1995). The art of case study research. Thousand Oaks, CA: Sage.
35. Staud, R. (2004). Fibromyalgia pain: do we know the source? Current Opinion in Rheumatology, 16(2), 157–163.
36. Staud, R. (2006). Are tender point injections beneficial: The role of tonic nociception in fibrom-yalgia. Current Pharmaceutical Design, 12(1), 23–27. http://dx.doi.org/10.2174/138161206775193235
37. Staud, R. (2007). Treatment of fibromyalgia and its symptoms. Expert Opinions on Pharma-cotherapy, 8(11), 1629–1642.
38. Staud, R. (2010). Pharmacological treatment of fibromyalgia syndrome: New developments. Drugs, 70(1), 1–14. doi:10.2165/11530950-000000000-00000
39. Turchaninov, R. (2000). Therapeutic Massage. A Scientific Approach. Phoenix, AZ: Aesculapius Books.
40. Turchaninov, R. (2006). Medical Massage (2nd ed.). Phoenix, AZ: Aesculapius Books.
41. Tylee, A., & Gandhi, P. (2005). The importance of somatic symptoms in depression in primary care. Primary Care Companion to the Journal of Clinical Psychiatry, 7(4), 167–176.
42. Van Houdenhove, B., & Egle, U. T. (2004). Fibromyalgia: The biopsychosocial piecing the puz-zle together. Psychotherapy and Psychosomatics, 73(5), 267–275. doi:10.1159/000078843
43. Vierck, C. J., Jr. (2006). Mechanisms underlying development of spatially distributed chronic pain (fibromyalgia). Pain, 124(3), 242–263.
44. Williams, D. A., & Arnold, L. M. (2011). Measures of fibromyalgia: Fibromyalgia Impact Ques-tionnaire (FIQ), Brief Pain Inventory (BPI), Multidimensional Fatigue Inventory (MFI-20), Med-ical Outcomes Study (MOS) Sleep Scale, and Multiple Ability Self-Report Questionnaire (MASQ). Arthritis Care & Research, 63(S11), S86–S97.
45. Wolfe, F., Clauw, D. J., Fitzcharles, M., Goldenberg, D. L., Katz, R. S., Mease, P.…Yunus, M. (2010). The American College of Rheumatology preliminary diagnostic criteria for Fibromyalgia and measurement of symptom severity. Arthritis Care & Research, 62(5), 600–610.
46. Yunus, M.B., Kaylan-Roman, U.P., Masi, A.T., Aldag, J.C. (1989) Electron Microscopic Studies of Muscle Biopsy in Primary Fibromyalgia Syndrome. A Controlled and Blinded Study. J. Reumat., 16(1)97-101
Category: Medical Massage
Tags: Issue #1 2016
