By Dr. Ross Turchaninov, Phoenix, AZ
With this article, we are finishing the discussion of a very important topic: the nature and role of Hyaluronic Acid (HA) in the function of soft tissues. Here are links to Part I and Part II, published in previous issues of the Journal of Massage Science:
There is a large gap between medical science, which has accumulated fascinating data about the clinical aspects of massage therapy, and the therapists and educators who are unaware of the solid scientific foundation of Medical Massage. As a result, desperate patients who are supposed to have full access to correct and efficient treatment options fall into this gap.
The main goal of SOMI’s educational project is to fill this gap and help Medical Massage be fully incorporated into mainstream medicine. The reason for this short introduction is the critical importance of the information we will discuss below for every therapist who practices clinical aspects of massage therapy.
Since I was a medical student, I have worked with patients in a clinical setting. I have researched and trained therapists on the entire concept of fascia rehabilitation, mainly targeting superficial connective tissue structures in the skin’s dermis and superficial fascia, which covers superficial skeletal muscles. However, recent research data indicates the opposite: the proper function of the soft tissues in each layer, including superficial fascia, is directly linked to the tension and scarification of the deep fascia, which separates the superficial and deep layers of skeletal muscles. For example, the proper function of the soft tissues in the posterior leg depends on the amount of tension built up in the deep fascia, which separates the gastrocnemius and soleus muscles.
This is a radical shift in our understanding of fascial tension, completely changing the dynamic of soft tissue therapies. There are several reasons for that, and we discussed them in Parts I and Part II. Revisiting this data will help readers with our discussion:
1. Deep fascia, a multilayered structure, is where special cells, such as fasciocytes, produce hyaluronic acid (HA). HA is primarily generated in the deep fascia (McCombe, et al., 2001), and it spreads to lubricate the superficial fascia, but secondarily.
2. HA is viscous and has a great affinity for water. Therefore, a combination of HA and water forms a fluid film between the soft tissue layers to properly lubricate the superficial and deep fascia and maintain normal gliding during muscle contractions.
3. Initial tension in the superficial fascia is a direct cause of dysfunction in the superficial skeletal muscles. However, tension in superficial fascia may or may not affect deep fascia (i.e., HA-producing stations) and deeply-located muscles. However, suppose the tension initially developed in the deep fascia (e.g., due to trauma or overload). In that case, it will always affect normal functions of the superficial fascia and superficially-located skeletal muscles.
4. The decline of HA production, decrease of HA viscosity, and eventually diminishing thickness of the HA+Water film are the first steps in forming adhesions between soft tissue layers. These adhesions are the real cause of all muscle dysfunctions except direct trauma. Therefore, we should stop endlessly chasing active trigger points and address superficial and especially deep fascia first before any muscle therapy even starts.
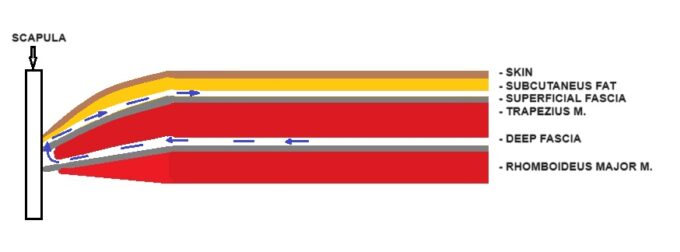
How does HA, which is generated in the deep fascia, contribute to the lubrication of the superficial fascia? Let’s look at Fig. 1, which represents the vertical arrangement of soft tissues in the middle back. Layers are indicated on the right, and insertion into the medial edge of the scapula is on the left. Typically speaking, there are narrow spaces between the fascia and the tissues above it, and these spaces are filled with fibrotic bridges that give soft tissues both mobility and stability at the same time. That is where the HA+Water film is located.
After HA generation, its molecules attract water and form an HA+Water film, which spreads along the fascia as fascial edges (Roman, et al., 2013). With the insertion of superficial and deep fascia into the periosteum (scapula in our case), their fibers are in direct contact with each other. The HA+Water film from the deep fascia eventually spreads into the superficial fascia, lubricating it. Blue arrows indicate the direction of HA-Water film flow in Fig. 1.
Re-Lubrication of the Deep Fascia
In Part II of this article, we discussed a limited set of clinical tools that therapists have to efficiently decompress superficial fascia (skin rolling, connective tissue massage, and mobile cupping with lifting component), and deep fascia (kneading with lateral shift). Now, we will discuss what therapists should do to re-lubricate fascia after decompression to restore the soft tissues’ normal function. This brings us to the fascinating study that Roman, et al. published in 2013 in the Journal of American Osteopathic Association. Let’s go over its main results in detail.
Since complex HA+Water is located between the soft tissue layers, scientists decided to examine whether lubrication between the layers of soft tissues behaves according to the Squeeze Film Lubrication Theory of fluid mechanics (SFLT). This theory mathematically describes the behavior of the fluid between two surfaces.
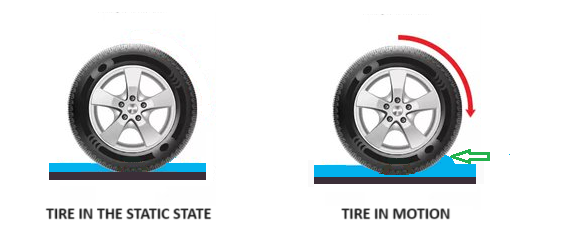
We regularly witness the work of SFLT around us. The most common example is how our cars’ tires behave when we are driving on wet roads in heavy rain. Everyone knows that cars are dangerously unstable on wet roads, and aggressive drivers can easily get into serious car accidents due to hydroplaning.
Let’s look at Fig. 2 and compare the events of two cars, looking at tires and very wet roads. One is in a static position, and the other is in motion on the wet road (Roman et al., 2013). The tires of a moving car on a wet road will behave according to the SFLT. In this case, the water pushed forward by the rotating tires creates a water wedge (green arrow), which is forced under the tires by further rotations, elevating them from the road. The more speed, the larger the water wedge, the more water gets under the tires, causing hydroplaning. As a result, tires lose traction with the road, the driver loses control of the car, and the accident happens.
Dr. Roman and his colleagues speculated that the HA+Water complex squeezed during manual strokes between layers of soft tissue should behave similarly to the water and tires on a wet road due to the same physics of SLFT. In both scenarios, normal lubrication lifts and separates soft tissue layers like tires on the road. Speed is a factor, as is the degree of pressure and its distribution. Thus, the study aimed to examine whether lubrication of fascia during manual therapy indeed follows the Squeeze Film Lubrication theory of fluid mechanics.
First of all, the authors establish five baseline scenarios between manual therapy and possible fascia lubrication:
- Constant sliding – repetitive horizontal sliding in one direction with a speed of 10 cm (4 inches) per second with a 150-degree angle. This is the approximate speed of slow effleurage strokes.
- Tangential Oscillation – vertical pressure with a back-and-forth oscillation stroke, staying in the same area.
- Back and Forth Sliding with 2 Hz frequency
- Back and Forth Sliding with 4 Hz frequency
- Perpendicular vibration – use of a mechanical massager to apply perpendicular vibrations to the superficial fascia, transmitted to the deep fascia. During vibration, the authors modulated the usage of:
- Low-frequency vibration 15-20 Hz
- High-frequency vibration around 60 Hz
Next, the authors used sophisticated mathematical tools to modulate possible relations between the therapist’s hands and the HA+Water film in the deep fascia. After mathematic models indicated that the HA+Water complex between the soft tissue layers should behave according to SFLT, the authors used Musculoskeletal Ultrasonography to observe relations between the therapist’s hands and the fluid film during massage strokes.
A very sensitive ultrasonograph produced images of the tiniest fluid layers, as small as 100 and 200 μm. This equipment allowed the authors to observe whether their mathematical models of fascia lubrication according to SFLT were correct.
RESULTS
Experimental data shows that the viscosity of HA significantly decreases when space between layers of the soft tissues diminishes, for example, due to muscle shortening. Additionally, we know that when pressure is applied to the superficial layers of the soft tissues, the thickness of the HA+Water film decreases. However, when the same pressure is released, the film’s thickness between the layers increases (Tadmor et al., 2002). The data we discuss below was obtained during a real-time ultrasound of different strokes using ultrasonography. Keeping this information in mind, let’s review the results of this fascinating study.
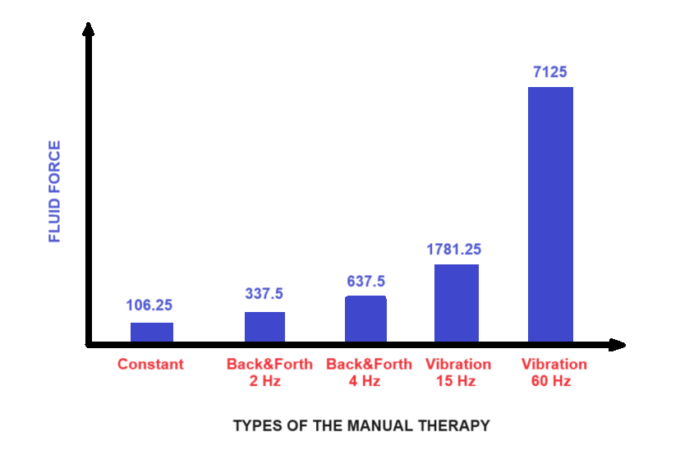
The diagram below (Fig. 3) recreates the study’s results conducted by Roman, et al. (2013). Each column presents the pressure peak within the HA+Water film when applying different strokes.
Explanation of Vibration Application (15 and 60 Hz)
Readers may see that applying perpendicular vibration with a frequency of 60 Hz produces the highest pressure and thickness within the HA+Water film. However, no water wedge is generated during vertical vibration, and the authors detected a fluctuation of the film pressure only in the vertical direction without its horizontal distribution. Conclusion: The largest HA+Water film but NO ‘water wedge’ were detected.
Explanation of Tangential Oscillation (2 and 4 Hz)
Tangential Oscillation, or back-and-forth strokes, produces moderate fluid pressure within the film. The more frequent the strokes, the more fluid force was detected. The authors also observed that the peak of pressure directly depended on the velocity of the strokes. Quicker strokes produce higher film pressure within fascial sheets. Conclusion: A slightly thicker HA+Water film and some ‘water wedge’ were detected.
Explanation of Constant Strokes
The minor pressure peak was detected during manual strokes in a constant regime when pressure was equally distributed during the stroke. Although strokes with constant pressure produce the lowest fluid pressure, they clearly demonstrate the presence of the ‘water wedge’ formed in front of the therapist’s hands.
It increases the fluid gap and, consequently, the space between layers of soft tissues. It improves the sliding system and allows muscles to contract efficiently. The best angle for forming a ‘water wedge’ is 150 degrees. Thus, strokes with constant pressure support HA distribution between the layers. Conclusion: The smallest HA+Water film but the LARGEST ‘water wedge’ were detected
Manual Decompression and Re-Lubrication of the Fascia
Let’s bring the fascinating results of this study into the treatment room. During a full-body massage session, if no tension in the soft tissues is detected, therapists manually deform the fascia, alternating pressure. As a result, the inner pressure and thickness of the HA+Water film fluctuate as well. These repetitive fluctuations are the major source of fascia lubrication, which helps the client’s tissues work efficiently with proper lubrication.
The situation is entirely different if the patient developed soft tissue tension or tissues were traumatized. In these scenarios, the HA+Water film’s volume and thickness decline or even disappear. Let’s adjust the manual therapy so we are not discussing the proper distribution of the HA+Water film but rather a restoration of HA production and fascia re-lubrication.
If we want to practice Medical Massage according to modern science rather than personal opinions, we should make the following adjustments to our therapy in our treatment rooms. After preparing the affected area (drainage, inhibitory regime of massage therapy, etc.), the therapist should first address the superficial and deep fascia before any muscle work.
In Part II, we discussed what therapists should do to decompress superficial and deep fascia to widen the space between soft tissues by locally stretching fibrotic bridges. This therapy allows us to mechanically stretch fibrotic bridges to increase space between soft tissue layers. Now, it is time to re-lubricate the deep fascia.
First Step: The therapist must decompress the superficial fascia (we discussed that in previous parts).
Second Step: The therapist must use lateral shift techniques to decompress the deep fascia (we discussed that in previous parts).
Third Step: The therapist must apply vertical electric vibration with 60 Hz in the fixed regime.
The massager must produce true vibration rather than vibration due to percussion. According to the authors, it will significantly increase the thickness of the HA+Water film locally in the deep fascia. It is better to apply vibration through a towel separating the massager and the skin.
After a minute of fixed vibration, the therapist should apply strokes with a 150-degree angle using the same pressure. The strokes must be applied in all directions, including against drainage. Each stroke must start from the fascia insertion into the periosteum of the bone and finish at the opposite point of the fascia insertion into the bone. This is a critical aspect since it allows the therapist to re-lubricate superficial fascia (see Fig. 1)
These strokes will increase inner fascial pressure, form a water wedge, and separate soft tissue layers like water elevates the car tires when we drive on a wet road. While lifting the upper layer of the soft tissues using a water wedge as a tool, the therapist additionally opens space between the outer and inner layers of the deep fascia. Decrease of intra-fascial pressure in the deep fascia frees fasciocytes, re-activating HA production and eventually re-lubricating the fascia.
To summarize fascia’s re-lubricating strokes applied AFTER the application of electric vibration:
1. The speed should be moderate, and a bi-manual application is preferable.
2. The therapist’s hands must be arranged at 150 degrees.
3. Stokes should be applied in different directions to form and use the water wedge as a tool.
4. Pressure must be equally distributed during strokes. Otherwise, the therapist loses the water wedge. To do that correctly, the therapist’s body must always be above his or her hands. If the therapist pushes their hands forward while the body stays behind, the pressure alters, and the water wedge is lost.
5. Each stroke starts and ends at the fascial insertions into the bone structures
The videos below illustrate strokes for fascia lubrication after applying electric vibration. The body mechanic is essential since the therapist must maintain equal pressure during stroke execution. The therapist must keep hands close to the body to do that.
For example, in both videos, fascia lubrication strokes are applied in the middle back to enhance lubrication of the deep fascia, separating the trapezius from the rhomboid muscles. Dots indicate tips of spinous processes of the thoracic vertebrae, while the dashed line is the medial aspect of the scapula. These two areas were superficial fascia, which covers the trapezius muscle and trapezius muscle itself; deep fascia, which covers rhomboids and separates them from the trapezius; and finally, rhomboids muscles inserted into the periosteum of the scapula and spinous processes.
Two lubricate deep fascia and, eventually, superficial fascia strokes must start at one bone structure (line of spinous processes) and finish at the other (medial edge of the scapula). Another equally important aspect is the placement of the contact area (thumbs in the video) under 150 degrees. This position gives the larger water wedge, which travels in front of the therapist’s hands, lubricating the fascia. Video 1 below illustrates the slow execution of strokes with 150 angles.
Lubricating the deep and eventually superficial fascia strokes that generate water wedges must be done in different directions, and this can be done quicker with bi-manual application.
HA SUPPLEMENTATION
After the publication of Parts I and II, therapists asked us about HA supplementation. Indeed, studies confirmed that taking HA helps the body to produce it. The commonly recommended daily dosage of HA from several sources (Tashiro et al., 2012; Sugiyama et al., 2024) is 200 mg once a day.
HA from two sources, Hyabest and Horbaach companies, was successfully tested in a clinical setting against a placebo. We share data without any financial interest. It is essential that each dosage of HA be taken with vitamin C. Finally, adding carrots, onions, turnips, and potatoes helps to increase HA production naturally.
SOMI’s Training
Consider joining SOMI on September 28-30 for Live Hands-on training in application of Medical Massage protocols (24 CEUs):
Saturday: Chronic Cervical Pain (Trapezius and Levator Scapulae Muscle Syndromes)
Sunday: TMJ Dysfunction. Positioning Vertigo
Monday: Soft Tissue Trauma. Leg Compartment Syndromes. Plantar Fasciitis
REFERENCES
McCombe, D., Brown, T., Slavin, J., & Morrison, W.A. (2001). The histochemical structure of the deep fascia and its structural response to surgery. Journal of Hand Surgery, British and European Volume, 26(2), 89-97.
Roman, M., Chaudhry, H., Bukiet, B., Stecco, A., & Findley, T.W. (2013). Mathematical analysis of the flow of hyaluronic acid around fascia during manual therapy motions. Journal of the American Osteopathic Association, 113, 600–610.
Sugiyama, K., Oe, M., Tanaka T., Matsuoka, R., Takeda, Y., Kimura, M., & Odani, K. (2024). Oral sodium hyaluronate relieves knee discomfort: A 12-week double-blinded, placebo-controlled study. Experimental and Therapeutic Medicine, Feb 27(2), 64.
Tadmor, R., Chen, N., & Israelachvili, J.N. (2002). Thin Film rheology and lubricity of hyaluronic acid solutions at a normal physiological concentration. Journal of Biomedical Materials Research, 61(4), 514-523.
Tashiro T., Seino, S., Sato, T., Matsuoka R., Masuda Y., & Fukui, N. (2012). Oral administration of polymer hyaluronic acid alleviates symptoms of knee osteoarthritis: A double-blind, placebo-controlled study over a 12-month period. Scientific World Journal, 167928.
Category: Medical Massage
Tags: 2024 Issue #2